Swelling, also known as edema, is a condition where fluid accumulates in the body's tissues, causing them to swell. It’s a frequent issue for people with diabetes, and understanding why it happens is essential for proper management.
High blood sugar levels can damage blood vessels, making it difficult for the body to circulate fluids properly. As a result, fluid can pool in different parts of the body, leading to swelling.
While swelling can affect various areas, people with diabetes often experience it in their legs, feet, and ankles. This is because blood circulation is already challenged in these areas, making them more susceptible.
Managing swelling involves a mix of lifestyle changes such as maintaining a healthy diet, regular exercise, and keeping blood sugar levels under control. Simple tips like elevating the feet and reducing sodium intake can also make a significant difference.
On the medical front, there are several treatments available, ranging from diuretics to specific medications prescribed by healthcare professionals. It's crucial to work closely with a healthcare provider to tailor a plan that suits individual needs.
- How Diabetes Causes Swelling
- Common Areas Affected by Swelling
- Managing Swelling with Lifestyle Changes
- Medications and Medical Treatments
How Diabetes Causes Swelling
Understanding the connection between diabetes and swelling starts with how high blood sugar levels affect the body. When blood sugar is persistently elevated, it can lead to damage in various organs and tissues, starting with the blood vessels. Over time, this damage can weaken blood vessels, making it difficult for the body to handle fluid balance properly, leading to swelling or edema.
The damage begins in the smallest blood vessels, called capillaries, which are crucial for delivering oxygen and nutrients to tissues. High blood sugar can cause these capillaries to become less permeable, which results in leaking of fluids into surrounding tissues. This fluid accumulation is what we see as swelling, mainly in the extremities such as the legs, ankles, and feet.
Another factor contributing to swelling in people with diabetes is poor circulation. High blood sugar levels can lead to atherosclerosis, a condition where plaque builds up in the arteries. This narrowing of the arteries restricts blood flow, making it harder for the body to circulate fluids effectively. In areas with already limited circulation, like the lower limbs, this difficulty can exacerbate fluid retention and swelling.
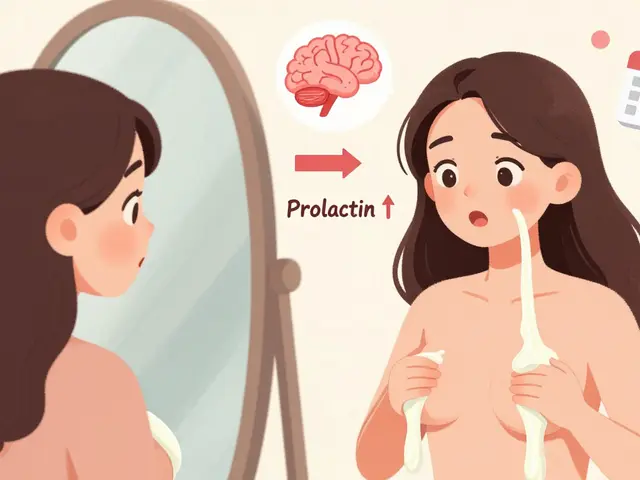
Mediating this swelling also involves the kidneys, which play a vital role in balancing fluids in the body. Diabetes can damage the kidneys, impairing their ability to filter blood and manage fluid levels properly. When the kidneys are not functioning well, they can contribute to fluid retention, leading to further swelling.
A significant aspect to consider is the role of insulin - the hormone responsible for regulating blood sugar. In type 2 diabetes, the body's cells become resistant to insulin. As a result, blood sugar levels remain high. This resistance can also affect how the body handles sodium, causing the kidneys to reabsorb more sodium than usual. Sodium retains water, which means more swelling. According to a study published in the Diabetic Medicine journal, close to 40% of patients with diabetes reported experiencing some level of swelling.
"Swelling in diabetic patients is often an indicator of underlying complications that require immediate attention and management," says Dr. John Wharton, a specialist in diabetic care.
The role of medications is another piece of the puzzle. Some drugs used to manage diabetes, such as thiazolidinediones, can cause fluid retention as a side effect. Patients need to be aware of these potential side effects and discuss with their healthcare providers to manage their condition effectively.
Recognizing the various contributing factors to swelling in diabetes is crucial for effective management. Ensuring good blood sugar control, monitoring blood pressure, maintaining a balanced diet low in sodium, and adhering to a regular exercise routine can help in reducing the risk of swelling. Additionally, routine check-ups with healthcare providers can catch any issues early and provide guidelines tailored to individual needs.
Common Areas Affected by Swelling
Living with diabetes often means being vigilant about various symptoms, and swelling is a prominent one. Swelling usually manifests in specific areas of the body, with some regions being more susceptible due to circulation issues and fluid retention challenges. Understanding where and why these swellings occur can help in taking proactive measures.
The most common areas where people with diabetes experience swelling are the legs, feet, and ankles. This happens because these parts of the body are farthest from the heart, making it harder for blood to return. High blood sugar levels can damage blood vessels and nerves, further complicating circulation.
Another area often affected is the hands. Those with diabetes might notice their rings feeling tighter or experience puffiness in the fingers. This can be particularly noticeable in the morning after a night's rest, as fluids settle during sleep.
While less common, the face can also experience swelling. This might not be as prominent as swelling in the legs, but some people do report puffiness around the eyes and cheeks, especially after periods of poor blood sugar control. Such swelling can sometimes be mistaken for other issues like allergies or infections.
According to Dr. Sarah Williams, an endocrinologist specializing in diabetes management, "Diabetic patients should pay close attention to any sudden or severe swelling, as it can indicate underlying complications like kidney issues or heart problems".
Swelling in the abdominal area can also be a concern. This isn't as commonly discussed but is important to note, especially if it comes with other symptoms like shortness of breath or drastic weight gain. It can point to fluid buildup in body cavities, needing immediate medical attention.
To manage swelling effectively, it's crucial to monitor these areas regularly. Simple habits such as removing socks and shoes at the end of the day and checking for imprints or marks on the skin can reveal early signs of edema. Elevating the legs periodically, especially after prolonged sitting or standing, can aid in reducing swelling.
If swelling persists or worsens, medical intervention might be necessary. Physicians can run specific tests to determine the cause and suggest appropriate treatments. Diuretics, which help the body get rid of excess fluid, are commonly prescribed. Moreover, other medications t managing blood sugar levels can alleviate and prevent swelling.
Managing Swelling with Lifestyle Changes
Managing swelling when you have diabetes can be effectively tackled through lifestyle changes. One of the first steps is to maintain a healthy diet. A diet low in sodium can help reduce fluid retention. Reducing processed foods and fast foods, which often have high salt content, can make a big difference. Instead, focus on eating fresh fruits, vegetables, and lean proteins.
Regular exercise is also crucial in managing swelling. Physical activity helps improve blood circulation, which can prevent fluids from pooling in the lower extremities. Activities like walking, swimming, or yoga are particularly beneficial. Engaging in at least 30 minutes of moderate exercise most days of the week can significantly improve symptoms.
Keeping blood sugar levels under control is another essential aspect. High blood sugar can damage blood vessels, leading to issues with fluid balance in the body. Monitoring your blood sugar levels regularly and adhering to your diabetes management plan prescribed by your healthcare provider is key. Consistent monitoring can prevent fluctuations that can aggravate swelling.
Another helpful practice is elevating your feet whenever possible. Elevation helps blood flow back to the heart and reduces the pooling of fluids. Try to elevate your feet above heart level for about 15-30 minutes a few times daily. This easy habit can lead to noticeable improvements in swelling.
Staying hydrated is important as well. While it may seem counterintuitive to drink more water if you're experiencing swelling, proper hydration helps your kidneys function better, which can reduce fluid retention. Aim to drink at least 8 glasses of water a day but adjust based on your body's needs and your doctor's advice.
Compression socks can also be a useful tool. These specialized socks apply gentle pressure to your legs, promoting better blood circulation and reducing swelling. It's vital to select the right size and compression level, so consulting with a healthcare provider for recommendations is a good idea.
Reducing alcohol consumption can also help. Alcohol can lead to dehydration and make your body hold onto more fluids. Limiting intake or abstaining can prevent additional swelling issues. Moreover, smoking can deteriorate blood vessel health, making swelling worse, so quitting smoking is highly beneficial.
Here's a quick checklist of lifestyle changes that can help manage swelling:
- Reduce sodium intake
- Engage in regular physical activity
- Monitor and control blood sugar levels
- Elevate your feet regularly
- Stay hydrated
- Wear compression socks
- Limit alcohol consumption
- Quit smoking
Remember, these lifestyle changes can significantly impact your quality of life and help manage swelling effectively. Consistency is key, and working closely with your healthcare provider can tailor these recommendations to fit your unique needs.
Medications and Medical Treatments
Addressing swelling in diabetes often requires medical interventions in addition to lifestyle changes. The most common approach involves the use of diuretics. Diuretics, often referred to as 'water pills,' help the kidneys remove excess salt and water from the body. This can significantly reduce fluid buildup and alleviate swelling.
Another key aspect is managing blood sugar levels through medications such as insulin or oral hypoglycemic agents. Keeping blood sugar levels stable can prevent further damage to blood vessels, which, in turn, can help reduce swelling. For some patients, combining these medications with angiotensin-converting enzyme (ACE) inhibitors can improve cardiovascular health and decrease fluid retention.
Anti-inflammatory medications may also be prescribed in cases where swelling is accompanied by inflammation. These drugs reduce inflammation and alleviate pain, contributing to a reduction in overall swelling. However, it's crucial to consult with a healthcare provider as some anti-inflammatory medications can have side effects or interact with other diabetes medications.
According to Dr. Sarah Bennett, a renowned endocrinologist, "Long-term management of diabetes-related swelling involves a multi-faceted approach that includes medications, lifestyle modifications, and regular monitoring by health professionals."
Another interesting treatment option involves the use of compression garments. Compression socks or stockings can help encourage blood flow and reduce fluid accumulation in the legs and feet. These garments are especially helpful for those who experience significant swelling in the lower extremities.
In more severe cases, hospitalization might be necessary where intravenous diuretics and other specialized treatments can be administered. This is often the case for patients who develop complications such as congestive heart failure or nephrotic syndrome, which exacerbate swelling. Physicians might also perform diagnostic tests such as ultrasound or MRI to ensure that no underlying conditions are causing the swelling.
Advanced Medical Treatments
Advanced treatments may include surgical options or procedures to address underlying issues contributing to edema. For instance, if a blockage in the lymphatic system is detected, surgical intervention might be needed to clear the obstruction. Some patients might also benefit from dialysis if their kidneys are significantly impacted and unable to manage fluid balance effectively.
Lastly, ongoing treatment plans are tailored to individual needs since the underlying causes and severity of swelling can vary greatly. Regular consultations with healthcare providers allow for adjustments in treatment strategies to better manage symptoms and improve quality of life.





Mirian Ramirez
I've been dealing with this swelling for years now, and honestly? The biggest game-changer was cutting out processed snacks. I used to think it was just aging, but nope-turns out my chips and frozen dinners were flooding my ankles. Now I snack on almonds and apple slices, and my shoes fit again. It’s not magic, just common sense.
Also, drinking water sounds weird when you’re swollen, but trust me-it helps. Your kidneys need it to flush out the sodium. I used to avoid it, thinking it’d make it worse. Big mistake. Now I drink a gallon a day and my legs don’t feel like lead weights by 5 PM.
Herbert Lui
Swelling isn’t just a symptom-it’s a whisper from your body saying, ‘Hey, you’ve been ignoring me for too long.’
Diabetes doesn’t just mess with sugar. It messes with rhythm. With flow. With the quiet hum of your veins trying to get home after a long day. When the capillaries leak, it’s not just fluid-it’s frustration. It’s time that’s been stolen. It’s the body’s poetry written in edema.
And yet-we still rise. We elevate. We walk. We drink. We care. That’s the real treatment. Not the pills. Not the socks. The stubborn, quiet act of showing up for yourself, even when your feet hurt.
Nick Zararis
Okay, let’s be clear: sodium is the enemy. No exceptions. No ‘but I like salty chips’-you’re not a child, you’re an adult with diabetes. You know better. Reduce it. Period. And don’t just say you’re ‘trying’-actually do it. Track it. Use an app. Write it down. Your kidneys are begging you.
Also-compression socks aren’t optional. They’re not ‘fancy leg accessories.’ They’re medical equipment. Wear them. Buy them. Don’t wait until your ankles look like overstuffed sausages. And elevate your feet-yes, even while watching TV. It’s not laziness-it’s self-care.
And for the love of all that is holy-stop drinking soda. I’m not joking. It’s sugar, sodium, and carbonation. Triple threat. You’re not hydrating. You’re poisoning yourself.
Rebecca Breslin
Ugh, I’m so tired of people acting like this is some mysterious medical mystery. It’s not. It’s basic biology. High sugar = damaged vessels = fluid leaks. End of story. You don’t need a PhD to understand this. You need to stop eating donuts and start walking.
Also, everyone keeps talking about diuretics like they’re some miracle cure. Newsflash: they just make you pee more. They don’t fix the root problem. You fix the root problem by controlling your blood sugar. That’s it. No magic pills. No ‘advanced treatments.’ Just discipline. And most people don’t have it.
And if you think compression socks are ‘uncool,’ you’re part of the problem. Wear them. Or don’t. But don’t come crying to me when your legs swell to twice their size.
Kierstead January
Let’s be real-this whole ‘swelling is from diabetes’ thing is just a distraction. The real issue? America’s food industry. They’ve been poisoning us with salt and sugar for decades. And now we’re paying for it with swollen ankles and kidney failure.
And don’t get me started on doctors. They push meds like they’re vending machines. ‘Take this pill, here’s another.’ But nobody asks: why are you eating that pizza at 2 a.m.? Why are you sitting all day? Why are you blaming the disease instead of your choices?
It’s not diabetes causing this. It’s laziness. And denial. And corporate greed. Fix the system. Or fix yourself. But stop pretending it’s just a medical glitch.
Imogen Levermore
Did you know the government has been secretly adding sodium to insulin to make people swell? 😏
Just kidding… maybe? 😅
But seriously-why do all the ‘experts’ ignore the fact that glyphosate in our food messes with capillary function? It’s not just sugar. It’s the chemicals. The EMFs. The 5G towers vibrating your lymphatic system. I’ve seen it in my own body. Swelling started the week I got my new phone. Coincidence? I think not. 🌐💧
Also, compression socks? Nah. I wear copper bracelets. They balance the biofield. And I drink lemon water with Himalayan salt. It’s all about frequency, baby. 🔮
Chris Dockter
Swelling is just your body saying you're lazy. Move. Eat less sugar. Done.
Gordon Oluoch
You people treat this like it’s a lifestyle blog. It’s not. It’s a slow, silent death sentence disguised as ‘edema.’
Every time someone says ‘just drink more water’ or ‘elevate your feet,’ I cringe. You’re treating symptoms like solutions. You’re not fixing the broken system. You’re not addressing the insulin resistance. You’re not confronting the fact that your pancreas is giving up and your kidneys are drowning.
And yet-you still eat the cake. You still skip the walk. You still ignore the numbers.
This isn’t about socks or sodium. It’s about accountability. And most of you? You don’t have it.
Tyler Wolfe
I’ve been diabetic for 12 years and I used to think swelling was just ‘part of it.’ Then I started walking 20 minutes after dinner-every night. No excuses. Even in the rain.
My ankles don’t puff up like balloons anymore. I still have bad days, but now I know: movement is medicine. Not just for the heart-for the feet too.
And hey-if you’re reading this and feeling overwhelmed? Start small. One day. One walk. One glass of water. You don’t need to fix everything today. Just start.
You’ve got this. I believe in you.
April Liu
When I first got diagnosed, I thought swelling meant I was failing. Like my body was betraying me.
Turns out-it was just trying to tell me something.
My mom used to say, ‘Your feet are your foundation.’ I didn’t get it until my ankles swelled so bad I couldn’t tie my shoes. Then I started wearing compression socks, drinking water like it was my job, and walking after every meal.
It’s not glamorous. No one posts about it on Instagram. But my legs don’t hurt anymore. And I sleep better.
And yes-I still eat chocolate. Just not every day. 😊
You’re not alone in this. I’m right here with you.
Emily Gibson
I love how this post breaks it down without being scary. A lot of medical stuff feels like a lecture, but this? This feels like a friend sitting with you, saying, ‘Hey, here’s what’s going on-and you’ve got options.’
For me, the biggest shift was realizing I didn’t have to be perfect. Just consistent. Some days I forget to elevate. Some days I eat too much salt. But I don’t beat myself up. I just reset the next day.
And I started keeping a little journal-just a note each night: ‘Walked? Yes.’ ‘Sodium under 1500? Mostly.’ It’s not fancy. But it helps.
Small steps. That’s all it takes.
Sara Mörtsell
People act like swelling is some new mystery but it’s been around since the dawn of processed food and insulin resistance. We’ve known this for decades. Why are we still pretending it’s complicated?
It’s not. Sugar damages vessels. Vessels leak. Fluid pools. End of story. The rest is just noise.
And don’t get me started on ‘natural remedies’ and ‘biofields’ and ‘copper socks’-you’re not healing your body, you’re wasting money.
Control blood sugar. Move. Reduce sodium. That’s it. No magic. No conspiracy. Just science. And discipline. And most people? They’d rather blame the moon than their breakfast burrito.
Rhonda Gentz
There’s something poetic about swelling, isn’t there?
It’s the body’s quiet rebellion. A refusal to be ignored. A slow tide rising in the feet, whispering: ‘You’ve been running from yourself.’
Diabetes doesn’t just affect blood sugar-it affects rhythm. The rhythm of breath. The rhythm of movement. The rhythm of care.
When we elevate our feet, we’re not just reducing fluid-we’re creating space. Space to breathe. Space to listen. Space to remember we’re not machines.
Maybe the real treatment isn’t the diuretic.
Maybe it’s the pause.
Alexa Ara
I was skeptical about compression socks at first. Thought they looked like grandma’s legwear. But after one week? My legs felt like they’d been given a hug.
And I started doing calf raises while brushing my teeth. Just 10 reps. No big deal. But it added up.
Also-cutting out soda was the hardest thing I’ve ever done. But the swelling? It went down within days. I didn’t even realize how much sugar I was drinking.
It’s not about being perfect. It’s about showing up. Even on the days you don’t feel like it.
You’re doing better than you think.
Olan Kinsella
You think this is just about your feet? No. This is about your soul.
Every time you eat that cookie, you’re not just spiking your sugar-you’re betraying your future self.
Every time you skip the walk, you’re telling your body you don’t care.
And now your ankles are swollen because you’ve been ignoring the whispers… until they became screams.
I’ve been there. I cried in the shower. I screamed at my glucose meter.
But then I chose to change.
Not because I had to.
Because I deserved better.
You do too.
Kat Sal
Okay real talk-I used to think swelling was just ‘water retention’ and I’d drink less water to fix it. Dumb. So dumb.
Turns out, dehydration makes it worse. Who knew?
Now I drink water, walk my dog every night, and I actually check my feet. Like, really look. Are there red marks? Are they shiny? Is it getting worse?
And I started using the MyFitnessPal app to track sodium. It’s a game-changer.
It’s not perfect. But I’m trying. And that’s enough for today.
Neil Mason
Just came back from Canada where my cousin with type 2 diabetes swears by soaking her feet in Epsom salt baths every night. Says it reduces swelling faster than anything.
Not sure if it’s placebo or science-but she’s been doing it for 8 years and her ankles look normal.
Also, in Canada we call them ‘compression stockings’ not ‘socks.’ Just saying. 😄
Anyway-glad this post is out there. So many people don’t realize how connected everything is. Blood sugar. Kidneys. Circulation. It’s all one system.
Andrea Gracis
I didn't know swelling could be from diabetes. I thought it was just being overweight. Thanks for explaining.
Matthew Wilson Thorne
Well-researched. Aesthetically pleasing layout. But the advice is pedestrian. Diuretics? Compression? Please. The real solution is intermittent fasting and ketosis. Everything else is just palliative care for the metabolically complacent.