A drug formulary is a list of prescription medications that your health insurance plan agrees to cover. It’s not just a catalog-it’s a tool that decides which drugs you can get at a lower price, and which ones might cost you a lot more-or not be covered at all. If you’ve ever been surprised by a high copay for a medication you thought was covered, you’ve run into the real-world impact of a formulary.
How a Drug Formulary Works
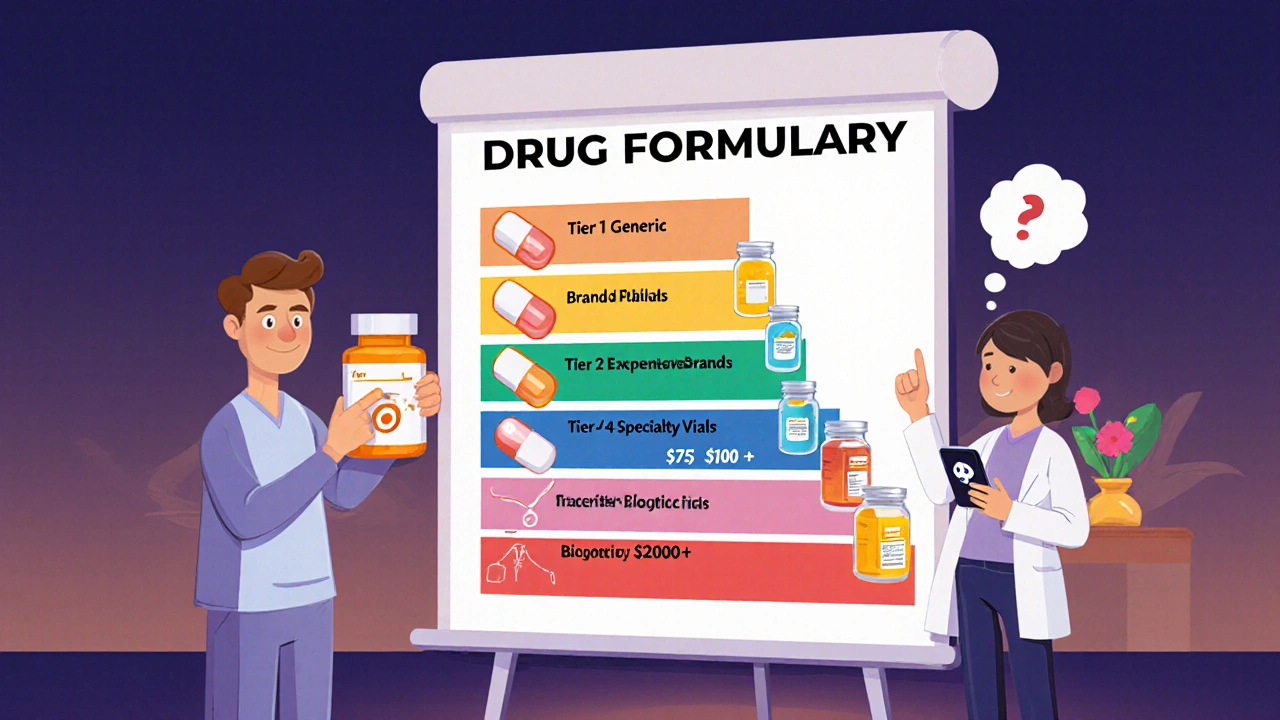
Think of a drug formulary like a menu at a restaurant. Not every dish is available, and some cost more than others. Insurance companies and Pharmacy Benefit Managers (PBMs) build these lists to balance two things: keeping you healthy and keeping costs manageable. They don’t just pick drugs randomly. A team of doctors, pharmacists, and researchers-called a Pharmacy and Therapeutics (P&T) committee-reviews every drug based on its safety, how well it works, and how much it costs. Only drugs that pass this review make the list.Most formularies are split into tiers. Each tier has a different price for you. The lower the tier, the less you pay. Here’s how it typically breaks down:
- Tier 1: Generic drugs - These are the cheapest. They contain the same active ingredients as brand-name drugs but cost far less. Most plans charge $0 to $10 for a 30-day supply.
- Tier 2: Preferred brand-name drugs - These are brand-name medications the plan favors because they’ve proven effective and cost-efficient. Your cost might be $25 to $50 per prescription.
- Tier 3: Non-preferred brand-name drugs - These are brand-name drugs that aren’t on the preferred list. You’ll pay more-often $50 to $100 per prescription.
- Tier 4: Specialty drugs - Used for complex conditions like cancer, rheumatoid arthritis, or multiple sclerosis. These can cost $100 or more per month, and sometimes you pay a percentage (like 30-50%) of the total cost.
- Tier 5: High-cost specialty drugs - Some plans have this level for the most expensive treatments, like certain gene therapies or biologics. Costs here can run into thousands per month.
These tiers aren’t the same across all plans. A drug that’s on Tier 2 in one plan might be on Tier 3 in another. That’s why switching insurance plans can suddenly make your medication much more expensive-even if the prescription hasn’t changed.
Why Some Drugs Aren’t on the Formulary
Not every drug you need will be on your plan’s list. When a drug isn’t included, it’s called “non-formulary.” This doesn’t mean it’s unsafe or ineffective. It just means your plan didn’t choose to cover it at a low cost. Maybe there’s a cheaper alternative that works just as well. Or maybe the drug is brand-new and hasn’t been reviewed yet.If your doctor prescribes a non-formulary drug, you might have to pay full price-sometimes hundreds or even thousands of dollars per month. That’s why it’s important to check your formulary before filling a new prescription.
But there’s a way out: you can ask for a formulary exception. Your doctor can submit a request explaining why you need this specific drug-maybe the alternatives didn’t work, caused side effects, or aren’t suitable for your condition. Most plans approve these requests. In 2023, about 67% of Medicare Part D exception requests were approved. For urgent cases, like a life-threatening condition, you can request an expedited review, which must be processed within 24 hours.
How Formularies Affect Your Health
Formularies aren’t just about saving money-they’re meant to help you get the best treatment. By encouraging the use of proven, cost-effective drugs, they reduce unnecessary spending and help avoid medications with poor safety records. Studies show that patients on formulary-approved drugs are more likely to stick with their treatment because they can afford it.But there’s a downside. Some patients get stuck in a cycle called step therapy. This means your plan forces you to try cheaper drugs first-even if your doctor says they won’t work for you. For example, you might need to try three different painkillers before your insurer will cover the one your doctor prescribed. This can delay treatment and cause unnecessary suffering.
Another issue is quantity limits. Your plan might only cover 30 pills a month, even if your doctor says you need 60. Or they might require prior authorization, meaning your doctor has to call or fill out paperwork before you can get the drug. These rules are meant to prevent waste, but they can be frustrating and time-consuming.

What You Can Do to Stay in Control
You don’t have to guess what’s covered. Here’s how to take charge:- Check your formulary before you fill a prescription. Most insurance plans post their full formulary online. Look for a link labeled “Drug List,” “Formulary,” or “Preferred Drugs.”
- Use tools like Medicare Plan Finder. If you’re on Medicare Part D, this free tool lets you enter your medications and compare plans based on your exact needs. It’s updated every October for the next year’s coverage.
- Ask your pharmacist. They have access to real-time formulary data and can tell you if your drug is covered and what your copay will be before you pay.
- Review your plan every year during open enrollment. Formularies change. A drug that was on Tier 2 last year might move to Tier 3-or be dropped entirely. Don’t assume it’s the same.
- Request a formulary exception if needed. If your drug isn’t covered and you can’t afford it, talk to your doctor about submitting an exception request. It’s your right.
In 2023, a Kaiser Family Foundation survey found that 68% of insured adults checked their formulary before filling a prescription. Those who did were far less likely to face surprise costs.
Recent Changes That Matter to You
In 2025, new rules are making formularies more patient-friendly:- Insulin is capped at $35 per month for all Medicare Part D plans. This started in 2023 and continues through 2025.
- Out-of-pocket caps on all drugs begin in 2025. Once you hit $2,000 in yearly costs for covered drugs, your plan pays 100% of the rest. This protects people on expensive treatments.
- Biosimilars are entering formularies. These are cheaper versions of biologic drugs (like Humira or Enbrel). As more are approved, expect lower prices for conditions like arthritis and Crohn’s disease.
- More transparency. Starting in 2025, plans must use standardized forms for exception requests, making the process clearer and faster.
These changes mean patients have more protection than ever. But you still need to stay informed. Just because a drug is covered doesn’t mean it’s affordable-or even available-on your plan.

Real Stories from Real Patients
One patient, ‘MedicareMom2023,’ shared on Reddit: “My diabetes drug moved from Tier 2 to Tier 3. My copay jumped from $35 to $85. I had to switch. It wasn’t my doctor’s first choice, but I couldn’t afford the old one.”Another, ‘CancerSurvivor87,’ said: “My immunotherapy was on Tier 4. I thought I’d pay $5,000 a month. My copay was $95. It saved my life.”
These stories show the same truth: formularies can be a lifeline-or a roadblock. It all depends on whether you know how to use them.
What to Do Next
Don’t wait until you’re at the pharmacy counter. Take five minutes now:- Go to your insurance website and find your formulary.
- Search for every prescription you take.
- Write down the tier and copay for each.
- If anything looks wrong or expensive, call your doctor or pharmacist.
Knowing your formulary isn’t just smart-it’s essential. It’s your key to avoiding surprise bills and getting the right meds at a price you can live with.
What is a drug formulary?
A drug formulary is a list of prescription medications that your health insurance plan covers. It’s organized into tiers that determine how much you pay out of pocket. The plan chooses which drugs to include based on safety, effectiveness, and cost.
Why is my medication not on the formulary?
Your medication might not be on the formulary because your plan considers it too expensive, has a cheaper alternative that works just as well, or hasn’t been reviewed yet. It doesn’t mean the drug is unsafe-it just means your plan doesn’t cover it at a low cost.
Can I get a drug that’s not on the formulary?
Yes. You or your doctor can request a formulary exception. You’ll need to explain why the drug is necessary-for example, if other drugs caused side effects or didn’t work. Many requests are approved, especially with strong medical justification.
Do formularies change every year?
Yes. Most plans update their formularies each January. Some changes happen mid-year too, but the plan must give you 60 days’ notice. Always check your formulary during open enrollment, even if you’re happy with your current plan.
What’s the difference between Tier 1 and Tier 2 drugs?
Tier 1 drugs are generics-the cheapest option. Tier 2 drugs are brand-name medications that your plan prefers because they’re effective and reasonably priced. You’ll pay more for Tier 2 than Tier 1, but less than for non-preferred brand drugs on Tier 3.
How do I find my plan’s formulary?
Log in to your insurance plan’s website and look for links like “Drug List,” “Formulary,” or “Prescription Benefits.” Medicare beneficiaries can use the Medicare Plan Finder tool at medicare.gov. You can also call your insurer or ask your pharmacist.
Are there any new rules about formularies in 2025?
Yes. Starting in 2025, Medicare Part D will cap your total out-of-pocket drug costs at $2,000 per year. After that, your plan pays 100%. Also, all plans must use simpler forms to request exceptions, making the process easier to understand.










Kaushik Das
Man, I never realized how much of a lottery this is. In India, we don’t have formularies like this-pharmacies just sell what’s available, and if it’s expensive, you pay or go without. But here? It’s like a corporate menu where your health is the appetizer and your wallet is the main course. I’ve seen people skip insulin because Tier 4 hit them with $400 a month. This system isn’t healthcare-it’s a profit algorithm with a stethoscope.
james thomas
Oh wow, so the ‘Pharmacy and Therapeutics Committee’ is just a bunch of suit-wearing bean counters pretending to be doctors? Classic. They don’t care about your kidneys-they care about the rebate the pharma company pays them to push certain drugs. I’ve seen Tier 2 drugs get demoted to Tier 3 the week after the CEO took a vacation in Bali. This isn’t medicine, it’s corporate espionage with pills.
Joe bailey
Love this breakdown! Seriously, so many people don’t know about the $2k out-of-pocket cap coming in 2025-that’s a game-changer for folks on biologics. And biosimilars? They’re the quiet heroes. My cousin’s rheumatoid arthritis meds dropped from $8K to $1.2K/month just because a biosimilar got added. Pharma’s scared, and honestly? Good. We’ve been getting ripped off for too long.
Amanda Wong
Wow. Just… wow. So now we’re supposed to be grateful because insulin is capped at $35? That’s barely a band-aid. The real crime is that these companies still charge $150+ in countries without price controls. And you call this ‘patient-friendly’? This isn’t reform-it’s PR. They’re just trying to look decent before the next election. Don’t be fooled.
Ezequiel adrian
Bro this is wild 😤 I just got my meds from Nigeria and paid $10 for a 90-day supply of metformin. Here? I pay $50 for 30 days and they act like it’s a gift. You people got a whole system built on making sick people feel guilty for needing help. 🤡
Sanjay Menon
Let’s be real-this entire formulary structure is a performative circus designed to make you feel like you’re in control while the real decision-makers sip lattes in New Jersey. I once had to wait 11 days for prior authorization on a drug my doctor said was ‘medically necessary.’ Meanwhile, the PBM executive got a $12M bonus. This isn’t healthcare. It’s a Ponzi scheme with pill bottles.
JAY OKE
I used to think formularies were just boring insurance stuff. Then my mom got diagnosed with MS and we found out her $12K/month drug was on Tier 5. We fought for a year to get it covered. Turns out, the ‘preferred’ alternative gave her seizures. We got the exception approved. She’s alive today because we knew to push. Don’t give up.
Stephen Adeyanju
My insurance moved my blood pressure med from tier 1 to tier 3 and now I'm paying $80 a month for something that used to be free I asked my doctor to switch but he said the other one makes me dizzy so I just skip doses now I'm fine
Asia Roveda
Of course the system is rigged. You think PBMs care about your health? They care about stock prices. And don’t even get me started on how these ‘exception requests’ are just a way to make you jump through hoops while they collect administrative fees. This isn’t a health system-it’s a tax on the sick. And Americans wonder why they’re broke.
Micaela Yarman
As a cultural liaison for immigrant patients, I’ve seen firsthand how devastating formulary changes can be. One elderly woman from Mexico cried because her diabetes medication was no longer covered-she’d been taking it for 12 years. She didn’t understand the tiers, didn’t speak English well, and was too proud to ask for help. We spent three weeks filing paperwork. She’s alive today because someone cared enough to fight for her. This isn’t just policy-it’s human dignity. Please, if you’re reading this: check your formulary. Not just for yourself-for the quiet ones who can’t speak up.