Standard Drink Calculator
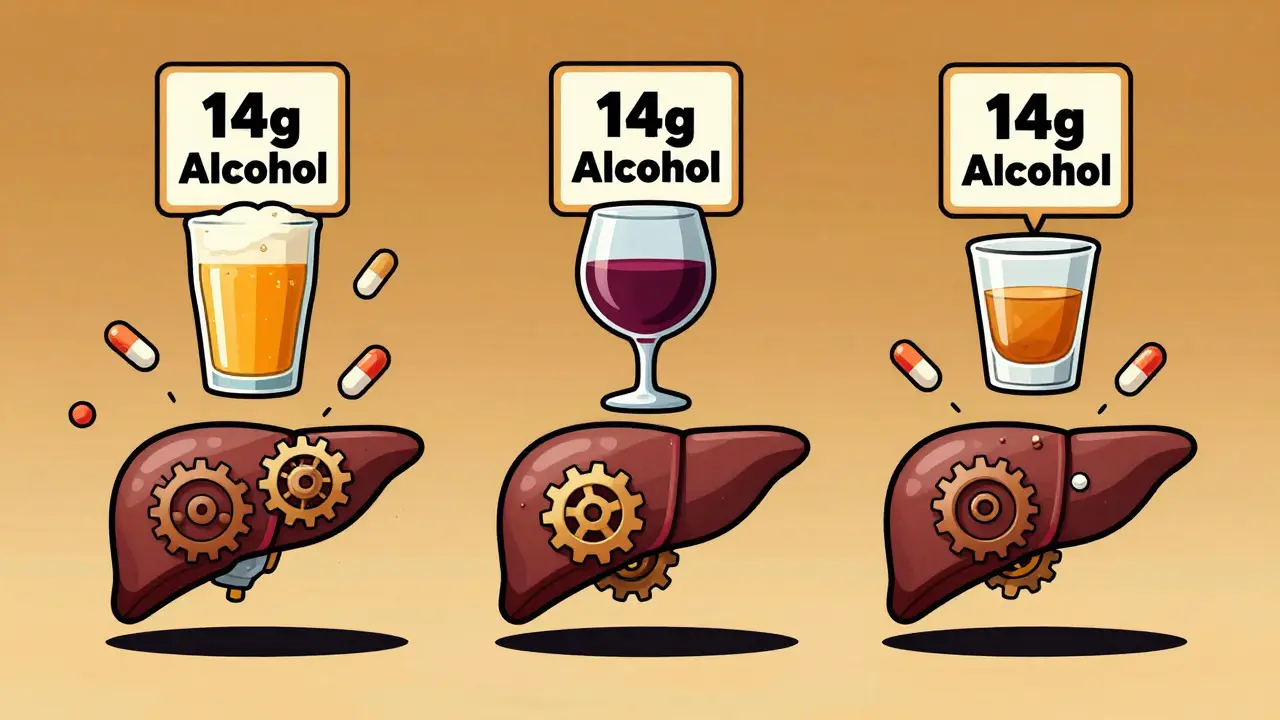
The article shows that all alcoholic beverages contain the same amount of pure alcohol per standard drink. 12 oz beer = 5 oz wine = 1.5 oz spirits = 1 standard drink (14g alcohol).
Your Alcohol Consumption
Important for medication safety: This calculator shows the total alcohol consumed. The article explains that all types of alcohol interact with medications the same way in your liver. Even one standard drink can be dangerous with certain medications.
Total standard drinks: 0
Total alcohol content: 0g
Recommended limit: 0 drinks
More than 40% of adults take prescription meds while drinking alcohol-often without realizing how dangerous it can be. It’s not about whether you sip wine, shoot whiskey, or crack open a beer. It’s about the alcohol inside-and how it fights your medicine for space in your liver.
One Drink, Same Risk-No Matter the Type
A 12-ounce beer, a 5-ounce glass of wine, and a 1.5-ounce shot of vodka all contain the same amount of pure alcohol: 14 grams. That’s one standard drink. And when it comes to how alcohol interacts with your medications, that’s the only number that matters.
It doesn’t matter if it’s light lager or aged bourbon. Your body breaks down ethanol the same way, no matter the source. The liver uses the same enzymes-alcohol dehydrogenase and aldehyde dehydrogenase-to process all of it. When those enzymes are busy with alcohol, they can’t do their job with your meds. That’s when things go wrong.
Take benzodiazepines, like Xanax or Valium. Mixing them with any alcohol-even one drink-can make you dangerously sleepy. Studies show this combo can increase sedation by 300% to 500%. That’s not just drowsiness. That’s slowed breathing, loss of coordination, even coma. And it happens just as fast with a glass of wine as it does with a shot of gin.
Why Spirits Feel More Dangerous (And Why They Are)
Spirits are often blamed for bad reactions. And for good reason. Emergency rooms see 68% of alcohol-medication overdose cases linked to spirits. But it’s not because spirits are chemically worse. It’s because they’re consumed faster.
Think about it: you sip wine slowly over an hour. You might have one or two glasses. But a shot of whiskey? That’s gone in five seconds. Your blood alcohol level spikes quickly. That rapid rise means your liver gets overwhelmed faster. Clinical trials show that when ethanol hits the bloodstream fast-like it does with spirits-the interaction with CNS depressants is 40% more severe than when the same amount is sipped slowly.
People think, “I only had one shot.” But that one shot delivers the same alcohol as a whole bottle of beer-just in a fraction of the time. That speed is what makes spirits riskier in real life, not because they’re more toxic.
Beer Isn’t Safe-It’s Just Easier to Overdo
Beer feels harmless. It’s low in alcohol. People say, “I had three beers, but they’re light.” But here’s the problem: you don’t stop at three. You keep going. And that’s where the danger hides.
The CDC says beer makes up 52% of total alcohol consumed in the U.S. That’s not because people drink more wine or spirits-it’s because beer is easy to drink in volume. And when you drink six or eight beers over a few hours, you’re hitting the same alcohol dose as four shots. That’s enough to interfere with painkillers, antidepressants, or blood thinners.
One common mistake? Taking ibuprofen with beer. People think, “It’s just beer.” But alcohol and NSAIDs like ibuprofen together irritate the stomach lining. Add them up over several drinks, and you’re looking at internal bleeding. In user reports, 63% of people who had stomach bleeding after mixing alcohol and NSAIDs were drinking beer.

Wine’s Hidden Risks-It’s Not Just the Alcohol
Red wine gets a bad rap for being “healthy,” but that doesn’t make it safe with meds. While the ethanol in wine acts the same as in beer or spirits, wine has other compounds that can interfere.
Red wine contains tannins and polyphenols-natural plant chemicals. One Mayo Clinic study found that red wine increased bleeding risk with warfarin by 15% compared to the same amount of ethanol from spirits. That’s because those plant compounds also thin the blood. So even if your alcohol dose is low, the combo with warfarin can push you over the edge.
And then there’s metronidazole. If you’re on this antibiotic, even a sip of wine can trigger a disulfiram-like reaction: flushing, rapid heartbeat, vomiting, chest pain. It’s not an allergy. It’s a chemical clash. The drug blocks alcohol breakdown, causing toxic acetaldehyde to build up. That reaction happens with any alcohol-but people think wine is “safer,” so they drink it anyway. That’s why 82% of reports about this reaction come from wine drinkers.
What About Non-Alcoholic Beer?
“It’s just 0.5% alcohol,” people say. “That can’t hurt.” But here’s the truth: even tiny amounts of alcohol can interfere with certain medications. If you’re on metronidazole, disulfiram, or some seizure drugs, 0.5% alcohol is enough to trigger a reaction.
A 2023 KFF survey found only 18% of adults know non-alcoholic beer still poses risks. That’s a dangerous gap. If your doctor says “no alcohol,” they mean zero. Not “almost zero.”
The Real Culprit: Blood Alcohol, Not the Bottle
Experts agree: it’s not the type of drink. It’s your blood alcohol concentration (BAC). A BAC of 0.05% from wine has the same effect on your liver and brain as a BAC of 0.05% from beer or vodka.
But here’s what’s missing from most warnings: timing. If you take your pill at 8 a.m. and have a drink at 8 p.m., you might think you’re safe. But many medications build up in your system. Alcohol can still interfere hours later.
For example, acetaminophen (Tylenol) and alcohol together are a silent killer. Just two standard drinks-any kind-increase your risk of liver damage by 300%. And that risk stays high for 24 hours after drinking. So even if you took your painkiller in the morning and had a drink at night, you’re still in danger.

What You Should Do
Here’s the bottom line:
- If your medication label says “avoid alcohol,” don’t drink anything-not beer, not wine, not spirits, not non-alcoholic beer.
- If you’re unsure, ask your pharmacist. They can check your exact meds and tell you if even one drink is risky.
- Use the standard drink rule: 12 oz beer = 5 oz wine = 1.5 oz spirits. Count your drinks this way, not by the glass or bottle.
- Don’t assume wine is “better.” It’s not. It’s just different.
- If you’ve had alcohol and feel dizzy, nauseous, or unusually tired after taking your meds, get help. Don’t wait.
What’s Changing in 2026
Hospitals and pharmacies are finally catching up. In 2023, the FDA approved new software that flags alcohol interactions by beverage type. By 2025, most electronic health records will warn doctors in real time if a patient drinks spirits while on opioids.
Medicare Part D now requires pharmacists to counsel patients on alcohol risks for 27 high-risk meds-including benzodiazepines, opioids, and antidepressants. And the CDC has made alcohol-medication interactions one of five top priorities for medication safety.
But technology won’t fix this unless people understand it. A 2023 NIH study showed patients who used visual drink charts improved their understanding of alcohol doses from 38% to 89%. That’s the real solution: clear, simple education-not fear.
Final Word
There’s no safe type of alcohol when you’re on meds. Not because one is worse than another. But because your body can’t handle the combo. The liver doesn’t care if it’s beer, wine, or whiskey. It just sees ethanol-and it’s already busy trying to process your pills.
When in doubt, skip it. Your body will thank you.
Can I have one drink with my medication?
If your medication label says "avoid alcohol," then no-even one drink can be dangerous. Many drugs, like benzodiazepines, blood thinners, and antibiotics, can have serious reactions with even small amounts of alcohol. Always check with your pharmacist before drinking.
Is red wine safer than beer or spirits with medications?
No. While red wine has antioxidants, it doesn’t make it safer with meds. In fact, its polyphenols can increase bleeding risk with warfarin, and it can trigger severe reactions with antibiotics like metronidazole. One standard drink of wine carries the same alcohol risk as a shot of vodka or a bottle of beer.
Does non-alcoholic beer count as alcohol with meds?
Yes. Non-alcoholic beer still contains up to 0.5% alcohol. For medications like metronidazole, disulfiram, or some seizure drugs, even that small amount can cause a reaction. If your doctor says "no alcohol," they mean zero.
Why do spirits cause more ER visits than wine or beer?
Spirits are consumed faster, leading to a rapid spike in blood alcohol levels. A 1.5-ounce shot delivers the same alcohol as 12 ounces of beer-but in seconds, not hours. That speed overwhelms the liver faster, making interactions with sedatives or painkillers more severe. It’s not the type of alcohol-it’s how fast you drink it.
How do I know if my medication interacts with alcohol?
Check the label for warnings like "avoid alcohol" or "may cause drowsiness." If it’s unclear, ask your pharmacist. They can look up your exact meds and tell you which ones are risky. Common high-risk categories include antidepressants, painkillers, sleep aids, antibiotics, and blood thinners.
What should I do if I accidentally mixed alcohol and medication?
If you feel unusually drowsy, dizzy, nauseous, or have trouble breathing, seek medical help immediately. Don’t wait. Call a poison control center or go to the nearest emergency room. Bring your medication bottle and tell them exactly what you drank and when.
Can I drink alcohol if I take my meds at different times of the day?
Sometimes, but not always. For drugs like acetaminophen, alcohol can still damage your liver even if you take them 12 hours apart. For others, like antidepressants, the drug stays in your system for days. The safest rule is to avoid alcohol entirely if your medication warns against it. Timing doesn’t eliminate the risk.




Shane McGriff
I used to think one glass of wine with my antidepressants was fine-until I passed out on the couch and woke up with my dog licking my face at 3 a.m. Turns out, my body doesn’t care if it’s Pinot or PBR. It just sees ethanol and gets confused. Now I just drink sparkling water with lime. My therapist says I’m ‘more present.’ I say I’m not hallucinating my cat singing opera anymore.
pragya mishra
You people are so dramatic. My uncle takes whiskey with his blood pressure meds every Sunday and he’s 82 and still drives his tractor. If you’re weak, don’t drink. Simple.
sagar sanadi
ALCOHOL IS A GOVERNMENT PLOT TO MAKE YOU SLEEPY SO YOU DON’T ASK QUESTIONS ABOUT THE FLUORIDE IN YOUR WATER. ALSO, THE FDA IS JUST A PHARMA FRONT. THEY WANT YOU TO THINK BEER IS SAFE SO YOU’LL KEEP BUYING IT AND NOT NOTICE THE MICROCHIPS IN THE CANS.
kumar kc
If you’re taking meds, don’t drink. Period. No excuses. You’re not special.
Renee Stringer
I read this article while sipping chamomile tea. It made me feel… responsible. I’ve been taking ibuprofen with beer for years. I didn’t realize it was slowly eating my stomach lining. I’ll stop. Not because I’m scared. Just… because it’s the right thing to do.
Thomas Varner
Okay, but… what about the guy who drinks one beer a week with his Zoloft? He’s fine. Like, physically fine. No ER visits. No blackouts. Just… a little more chill than before. Maybe it’s not about the alcohol? Maybe it’s about the person? Like, maybe some bodies just handle it? I’m not saying it’s safe… just… maybe it’s not a universal rule? Like, I dunno, maybe the liver has a personality?
Emily Leigh
So… let me get this straight… the real villain here isn’t alcohol… it’s… capitalism? Because if Big Pharma didn’t make us so anxious, we wouldn’t need meds… and if they didn’t make us so tired, we wouldn’t drink… so… it’s all their fault? And also, non-alcoholic beer is a scam? I’m not mad… I’m just… disappointed. And also, I’m gonna have a seltzer now. Because I’m woke.
Jacob Cathro
So let me decode this for the uneducated: alcohol + meds = liver meltdown. But here’s the kicker-your liver’s got a 12-hour shift, and if you hit it with ethanol at 8 p.m., it’s still on the clock at 2 a.m. trying to detox your Xanax. And you think you’re ‘safe’ because you ‘waited’? Nah. You’re just a walking tox lab. And yeah, non-alcoholic beer? Still got enough ethanol to trigger a disulfiram reaction like it’s a horror movie. Also, ‘one drink’ is a myth. You don’t have one. You have three. And then you blame the ‘spirits.’ Lmao.
Manoj Kumar Billigunta
I’ve worked as a pharmacist for 18 years, and I’ve seen too many people assume their drink is ‘fine’ because it’s ‘light’ or ‘natural.’ The science is clear: ethanol is ethanol. Whether it’s from a $200 bottle of red or a $2 six-pack, your liver doesn’t care. I tell my patients: if your doctor says no alcohol, treat it like a no-fly zone. One sip isn’t worth a hospital stay. And if you’re unsure? Call your pharmacy. We’re here to help-not judge.
Andy Thompson
USA 4 LIFE. If you’re on meds and still drinking, you’re weak. Real Americans don’t need booze to cope. We got guns, freedom, and hard work. Also, non-alcoholic beer? That’s a liberal trick to make you think you’re being healthy. It’s still poison. Drink water. Or don’t drink at all. America doesn’t need drunk patients.