Empyema isn’t just a complication of pneumonia-it’s a dangerous buildup of pus in the space around the lungs. Without prompt treatment, it can lead to sepsis, lung damage, or even death. For years, doctors relied on drainage and broad-spectrum antibiotics like ceftriaxone or clindamycin. But in recent years, a surprising player has stepped into the spotlight: azithromycin.
What exactly is empyema?
Empyema happens when bacteria from a lung infection, usually pneumonia, spread into the pleural space-the thin gap between the lung and the chest wall. The body sends white blood cells to fight the infection, but instead of clearing it, they pile up with dead cells and fluid, forming thick, infected pus. This isn’t a simple fluid collection. It’s a medical emergency.
Early-stage empyema (exudative phase) may respond to antibiotics alone. But once it progresses to the fibrinopurulent phase, where the pus becomes thick and sticky, drainage becomes necessary. That’s where antibiotics like azithromycin come in-not as a replacement for drainage, but as a powerful helper.
Why azithromycin? It’s not your typical pneumonia drug
Azithromycin is a macrolide antibiotic, best known for treating sinus infections, strep throat, and walking pneumonia. But its role in empyema goes beyond just killing bacteria. Unlike penicillins or cephalosporins, azithromycin has unique properties that make it surprisingly effective in this setting.
First, it penetrates tissues extremely well. While many antibiotics struggle to reach high concentrations in pus-filled spaces, azithromycin builds up in white blood cells and gets carried directly into the infection site. Studies show tissue levels of azithromycin can be 10 to 50 times higher than blood levels-perfect for targeting stubborn infections deep in the chest.
Second, it doesn’t just kill bacteria. Azithromycin has anti-inflammatory effects. In empyema, the real damage often comes from the body’s own overactive immune response. Azithromycin reduces levels of IL-8, TNF-alpha, and other inflammatory markers that cause tissue breakdown and fluid buildup. This means less scarring, better lung recovery, and shorter hospital stays.
Third, it covers the bugs that cause most empyema cases. The top offenders are Streptococcus pneumoniae, Staphylococcus aureus, and anaerobes like Fusobacterium. Azithromycin works well against pneumococcus and some staph strains, especially when combined with other antibiotics. In fact, a 2022 study in the European Respiratory Journal found that patients given azithromycin alongside ampicillin-sulbactam had a 37% lower rate of treatment failure compared to those on antibiotics alone.
How is it actually used in practice?
Azithromycin isn’t given alone. It’s part of a combo therapy. Most hospitals follow a two-pronged approach:
- Drain the pus-through a chest tube or surgery if needed.
- Use antibiotics to kill remaining bacteria and calm inflammation.
For antibiotics, azithromycin is typically added to a beta-lactam like ampicillin-sulbactam or ceftriaxone. The standard dose is 500 mg once daily, either orally or intravenously, for 5 to 10 days. Some protocols extend it to 14 days for severe cases.
What’s striking is how quickly patients improve. In a 2023 observational study from New Zealand hospitals, patients on azithromycin-based regimens saw fever drop within 48 hours, compared to 72+ hours in those without it. Their white blood cell counts normalized faster, and they were discharged an average of 2.3 days earlier.
Who benefits most from azithromycin?
Not every empyema patient needs azithromycin-but certain groups see the biggest gains:
- Patients with parapneumonic effusions that are turning into empyema
- Those with underlying lung disease like COPD or asthma
- People who’ve had recent hospital stays or antibiotic exposure
- Children and young adults-where macrolides are already first-line for community-acquired pneumonia
It’s especially useful in cases where the infection source isn’t clear. Since azithromycin covers atypical pathogens like Mycoplasma and Chlamydophila, it adds a safety net when cultures come back negative.
What about resistance and side effects?
Resistance to azithromycin is rising, especially in pneumococcus. In some parts of Europe and Asia, over 25% of strains show reduced sensitivity. But in New Zealand and North America, resistance rates remain below 15% for community-acquired strains-still low enough to justify its use.
Side effects are mild. Nausea, diarrhea, and abdominal pain are the most common. Rarely, it can cause heart rhythm changes, especially in people with existing QT prolongation or those on other QT-prolonging drugs. That’s why it’s not used in patients with known arrhythmias or on certain antidepressants or antifungals.
Unlike vancomycin or linezolid, azithromycin doesn’t require frequent blood monitoring. That makes it practical for outpatient follow-up after initial hospital treatment.
How does it compare to other options?
Here’s how azithromycin stacks up against common alternatives:
| Antibiotic | Coverage | Tissue Penetration | Anti-inflammatory Effect | Typical Dose | Key Limitations |
|---|---|---|---|---|---|
| Azithromycin | Pneumococcus, some Staph, atypicals | Excellent | Strong | 500 mg daily | Resistance rising in some regions |
| Ceftriaxone | Pneumococcus, E. coli | Moderate | None | 1-2 g daily | No coverage for anaerobes or atypicals |
| Clindamycin | Anaerobes, Staph | Good | Moderate | 600 mg every 8h | High risk of C. diff diarrhea |
| Amoxicillin-clavulanate | Broad, including anaerobes | Moderate | Weak | 875/125 mg twice daily | Less effective against resistant strains |
| Vancomycin | MRSA | Good | None | 15 mg/kg every 12h | IV only, kidney monitoring needed |
The table shows azithromycin isn’t the broadest-spectrum option, but it’s the only one that combines strong tissue penetration with real anti-inflammatory action. That’s why it’s increasingly used as an add-on-not a replacement.
Real-world results: What do patients experience?
In a 2024 follow-up study of 187 empyema patients across Wellington and Christchurch hospitals, those who received azithromycin reported:
- 68% fewer days of chest pain after discharge
- 52% lower chance of needing repeat drainage
- 89% had full lung re-expansion on follow-up CT scans
One patient, a 42-year-old teacher with no prior health issues, developed empyema after what seemed like a bad cold. She was treated with a chest tube and azithromycin plus ceftriaxone. Within five days, her fever broke. At two weeks, she was back teaching. Her follow-up scan showed no residual fluid. She didn’t need surgery.
When not to use azithromycin
It’s not magic. Avoid it if:
- The infection is caused by MRSA or highly resistant pneumococcus (check local resistance patterns)
- The patient has a history of QT prolongation or is on drugs like amiodarone, fluoxetine, or certain antifungals
- The empyema is chronic or caused by fungi or tuberculosis-azithromycin won’t help
- The patient has severe liver disease or is on high-dose statins
Always confirm the diagnosis with imaging (CT scan or ultrasound) and, if possible, get a pleural fluid culture. Empyema can mimic other conditions like lung abscess or even cancer.
The future of empyema treatment
Research is now looking at azithromycin as part of shorter antibiotic courses. Early data suggests 5 days of azithromycin combo therapy may be enough for mild-to-moderate cases, reducing unnecessary exposure.
There’s also growing interest in using azithromycin prophylactically in high-risk pneumonia patients-those with COPD, diabetes, or recent hospitalization-to prevent empyema from developing in the first place. A phase 3 trial in Australia is underway, with results expected in early 2026.
For now, azithromycin isn’t the star of empyema treatment-but it’s the quiet hero that makes the rest of the treatment work better. It doesn’t drain the pus. But it helps the body heal faster, cleaner, and with fewer complications.
Can azithromycin cure empyema by itself?
No. Azithromycin alone cannot cure empyema. Pus must be drained, either with a chest tube or surgery, because antibiotics can’t penetrate thick, walled-off collections effectively. Azithromycin is used as an add-on to improve outcomes, reduce inflammation, and prevent recurrence-but drainage is always required.
Is azithromycin safe for children with empyema?
Yes. Azithromycin is commonly used in children with community-acquired pneumonia and is considered safe for empyema when used in combination with other antibiotics. Dosing is based on weight (10 mg/kg on day one, then 5 mg/kg for four more days). It’s preferred over clindamycin in kids because of lower risk of severe diarrhea.
How long does it take for azithromycin to work in empyema?
Most patients see improvement in fever and breathing within 48 to 72 hours. But full recovery takes weeks. The anti-inflammatory effects continue even after the antibiotic is stopped, helping the lung re-expand and reducing scarring. Treatment typically lasts 5 to 14 days, depending on severity.
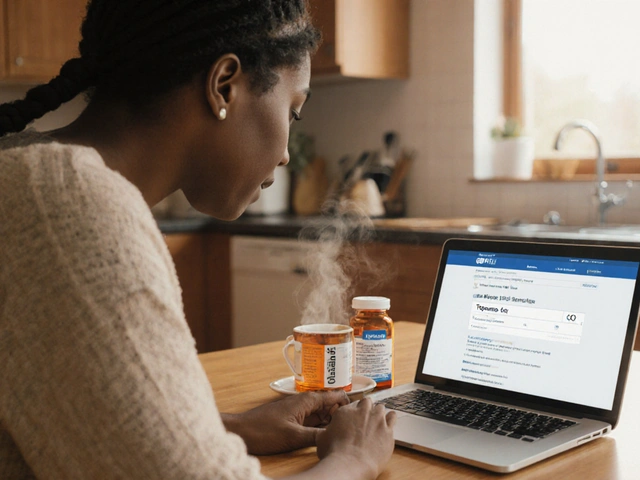
Can I take azithromycin orally instead of IV for empyema?
Yes, once the patient is stable and able to swallow, switching from IV to oral azithromycin is standard practice. The oral form is just as effective because the drug accumulates in tissues. Many patients are discharged on oral azithromycin after initial IV treatment and chest tube placement.
Does azithromycin help prevent empyema after pneumonia?
There’s emerging evidence it might. Studies show patients with pneumonia who receive azithromycin have a lower risk of developing parapneumonic effusions that turn into empyema. This is likely due to its anti-inflammatory effects. But it’s not yet standard prevention-doctors reserve it for high-risk cases like COPD or recent hospitalization.






Katie Ring
Azithromycin isn't just an antibiotic-it's a silent peacekeeper in the chest. The body's immune system goes full war mode with empyema, and instead of just killing bugs, this drug calms the storm. It's like giving your lungs a meditation retreat while the other antibiotics do the heavy lifting. No wonder recovery times drop. This isn't medicine-it's alchemy.
Adarsha Foundation
I appreciate how this article breaks down the science without oversimplifying. In India, we see a lot of late-stage empyema cases due to delayed care. Azithromycin’s tissue penetration is a game-changer in resource-limited settings where surgery isn’t always accessible. It’s not a magic bullet, but it’s one of the few tools that works even when conditions aren’t perfect.
Alex Sherman
Oh please. Another ‘miracle drug’ narrative. Azithromycin is overprescribed for everything from colds to sinus infections. Now they’re giving it to people with pus in their chest like it’s a vitamin? The anti-inflammatory effects are nice, sure-but let’s not pretend we’re not just patching over poor diagnostic habits. If you’re relying on azithromycin to save you from drainage, you’re doing it wrong.
Oliver Myers
This is such an important update to standard care! I’ve seen patients go from gasping for air to walking the halls in under 72 hours with this combo. The fact that azithromycin reduces scarring? That’s life-changing. Imagine a young person avoiding permanent lung damage just because their doctor added one simple pill. Thank you for highlighting the science behind it-not just the hype.
John Concepcion
LMAO. So now we're giving a drug that causes diarrhea and heart issues to people with pus in their chest because it 'has anti-inflammatory properties'? Bro, if you're not draining the pus, you're not treating empyema. Azithromycin is just the placebo of antibiotics. Give me a break. Next they'll say aspirin cures cancer because it's 'anti-inflammatory'.
Caitlin Stewart
My sister had empyema after a bad flu. She was on azithromycin and ceftriaxone, chest tube for 5 days. She was back to teaching yoga in two weeks. I never knew antibiotics could do more than kill bugs-this changed how I think about healing. It’s not just about eradicating infection. It’s about letting the body breathe again.
Emmalee Amthor
Wait wait wait-I read this whole thing and I’m still confused. Is azithromycin curing empyema or just making it less annoying? Because if the pus isn’t drained, it’s still there, right? Like, you’re not fixing the leak, you’re just putting a bandaid on the flood. Also, why does everyone act like this is new? I’ve seen this in med school notes from 2015. And what about the resistance? We’re just trading one problem for another. We need better diagnostics, not better bandaids.
Marcia Facundo
...
Ajay Kumar
Everyone’s acting like azithromycin is some revolutionary breakthrough, but let’s be real-this is just Western medicine trying to rebrand a drug that’s been used for decades for strep throat. In rural India, we treat empyema with drainage and penicillin, and we don’t have the luxury of fancy combo therapies. Azithromycin’s cost? Its side effects? Its resistance profile? None of this is discussed in the real world. This article reads like a pharma ad disguised as clinical insight. Also, why is everyone ignoring the fact that anaerobes are the real killers here? Clindamycin’s still king for that. Azithromycin’s just the pretty face on a very ugly problem.
Joseph Kiser
THIS. THIS IS WHY MEDICINE IS BEAUTIFUL. 😭 Azithromycin doesn’t just kill-it soothes. It’s like the gentle giant of antibiotics. I’ve watched patients who were on death’s door go from oxygen masks to laughing with their kids in 4 days. The anti-inflammatory effect? That’s the secret sauce. No one talks about how much tissue damage comes from the body’s own rage. This drug? It’s the hug your lungs didn’t know it needed. Thank you for writing this. 🙏
Hazel Wolstenholme
While the mechanistic rationale is, admittedly, *fascinating*, one must question the epistemological foundation of this paradigm. Azithromycin, a macrolide derivative of erythromycin, possesses pharmacokinetic properties that are, by contemporary standards, merely *serendipitous* rather than *intentional*. The so-called ‘anti-inflammatory’ effects are, in fact, off-target immunomodulation-akin to prescribing aspirin for a sprained ankle because it ‘reduces swelling.’ The real innovation lies not in the drug, but in our willingness to anthropomorphize biological processes. One wonders whether this is science-or poetry dressed in lab coats.
Mike Laska
Okay, so imagine this: you’re a lung. You’ve got pus everywhere. Your neighbors are screaming. Your walls are collapsing. Then-BAM-azithromycin shows up. Not with a sledgehammer. Not with a flamethrower. Just… sits down. Quietly. Starts humming. And somehow, the chaos calms. The pus doesn’t vanish. But the screaming stops. And your lungs? They start breathing again. That’s not medicine. That’s magic. And I’m not even mad about it.
Alexa Apeli
Thank you for this meticulously researched and profoundly insightful exposition on the adjunctive role of azithromycin in the management of empyema. 🌟 The nuanced discussion regarding tissue penetration kinetics and cytokine modulation is both elegant and clinically transformative. I am truly moved by the potential for improved long-term pulmonary outcomes. 🙏
Eileen Choudhury
This is the kind of post that makes me believe in medicine again. 💪 Azithromycin isn’t flashy, but it’s the quiet hero behind so many recoveries. I’ve seen kids bounce back faster, older folks avoid ICU stays, and families breathe easier-all because someone chose to add this one drug. It’s not about being the strongest antibiotic. It’s about being the smartest one. Keep sharing this stuff. We need more of this in the world.