Isoniazid Liver Risk Calculator
Assess Your Personal Risk
This tool estimates your risk of liver injury while taking isoniazid based on factors discussed in the article.
When you’re prescribed isoniazid for tuberculosis-whether you’re treating an active infection or preventing latent TB from flaring up-you’re getting one of the most effective drugs ever made for this disease. But here’s the catch: isoniazid doesn’t just fight TB. It also messes with your liver, and it doesn’t do so quietly.
Why Isoniazid Hits Your Liver Hard
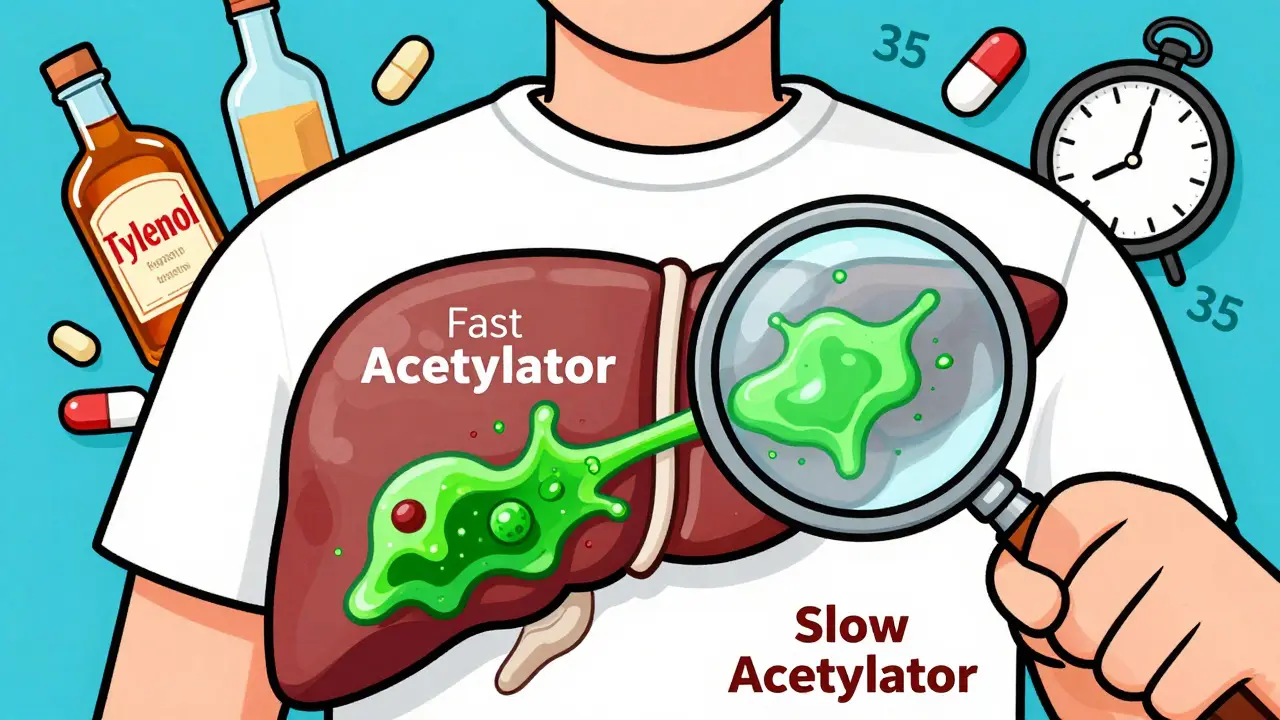
Isoniazid has been around since the 1950s, and it still works. But its power comes with a price. About 20 to 25% of people taking it show signs of liver stress, according to a 2016 study of 85 TB patients. That’s not rare. That’s common. And it’s not random. It’s tied to your genes. Your body breaks down isoniazid using an enzyme called NAT2. Some people have a version of this enzyme that works slowly-called slow acetylators. In Europe and North America, 40 to 70% of people fall into this group. In South Africa, it’s as high as 87%. These people don’t clear isoniazid fast enough. The drug lingers. And as it breaks down, it turns into toxic byproducts that attack liver cells. The result? Liver enzymes like ALT and AST spike. You might feel nauseous, tired, or have right-side abdominal pain. Jaundice-yellow skin or eyes-means things are getting serious. In most cases, the damage is mild and reversible if caught early. But in 30% of cases, it’s severe enough to stop treatment.It Gets Worse When Combined
Most people don’t take isoniazid alone. They take it with rifampin and pyrazinamide in a 2-month combo called HRZE. Sounds efficient. But here’s the problem: rifampin makes isoniazid’s liver damage worse. Rifampin turns on liver enzymes-CYP3A4 and CYP2E1-that speed up the breakdown of isoniazid into acetylhydrazine, a known liver toxin. Think of it like turning up the heat on a stove that’s already burning too hot. The result? A 5 to 15% chance of liver injury with combination therapy, compared to just 2 to 5% with isoniazid alone. Pyrazinamide adds fuel to the fire. The CDC says the full HRZE regimen carries a 10 to 20% risk of liver damage. That’s nearly one in five people. That’s why some clinics now use shorter 4-month regimens with rifampin and isoniazid only (HR), cutting the risk by nearly half. And here’s the twist: isoniazid doesn’t just hurt the liver on its own. It also messes with other drugs. It blocks liver enzymes that break down seizure medications like phenytoin and carbamazepine. That means those drugs can build up in your blood to dangerous levels-by as much as 57%. If you’re on any of these, your doctor needs to know.Who’s at Highest Risk?
Not everyone reacts the same way. Your risk depends on three things: your genes, your habits, and your health.- Slow acetylators: If your NAT2 gene makes you a slow metabolizer, your risk jumps 2.6 to 4 times higher. That’s the biggest factor.
- Alcohol use: Drinking more than 14 drinks a week for men, or 7 for women, triples your risk. Alcohol and isoniazid both stress the liver. Together, they’re a bad mix.
- Age: People over 35 are more likely to have serious liver damage. Older livers don’t recover as easily.
- Pre-existing liver disease: If your ALT is already over 3 times the normal level before you start isoniazid, you shouldn’t take it.
- Malnutrition or diabetes: These conditions make you more likely to get nerve damage from isoniazid, too.
What You Should Watch For
Most liver damage shows up quietly. You might feel fine. That’s why monitoring matters. The CDC and American Thoracic Society say: get baseline blood tests before starting isoniazid. Then check liver enzymes every month. But don’t wait for your appointment if you feel off. Symptoms to never ignore:- Nausea or vomiting that won’t go away
- Dark urine, like tea or cola
- Clay-colored stools
- Yellow skin or eyes
- Fever without a cold
- Unexplained fatigue or loss of appetite
How to Protect Yourself
You can’t change your genes. But you can take steps to reduce the risk.- Take vitamin B6 (pyridoxine): Every single person on isoniazid should take 25 to 50 mg daily. It prevents nerve damage, which affects up to 20% of users-and up to 50% of slow acetylators.
- Avoid alcohol: No exceptions. Even a few drinks a week can push you over the edge.
- Don’t take other liver-stressing drugs: Avoid acetaminophen (Tylenol) unless absolutely necessary. Even at normal doses, it adds to the burden.
- Get tested if you can: In Europe, some clinics test for NAT2 status before starting isoniazid. It’s not routine everywhere, but if you’re high-risk, ask your doctor. It could save your liver.

New Options Are Coming
The good news? We’re moving away from relying so heavily on isoniazid. The WHO now recommends a 4-month regimen using rifapentine and moxifloxacin for drug-susceptible TB. It cuts isoniazid exposure from 6 to 9 months down to just 4. That could reduce liver damage by 30 to 40%. For drug-resistant TB, a new combo called BPaLM (bedaquiline, pretomanid, linezolid, moxifloxacin) doesn’t use isoniazid at all. It’s a game-changer for people who can’t tolerate it. And research is looking at natural protectants. One 2021 study found milk thistle (silymarin) reduced liver injury by 27% in people taking isoniazid. It’s not standard yet-but it’s promising.The Bigger Picture
Tuberculosis still kills over 1.6 million people a year. Isoniazid is cheap-just 3 cents a pill in poor countries-and it works. That’s why it’s still used in 95% of TB regimens worldwide. But in places with better healthcare, doctors are already shifting. They’re using shorter courses. They’re testing for liver risk. They’re avoiding isoniazid in high-risk patients. The future isn’t about throwing out isoniazid. It’s about using it smarter. Knowing who’s at risk. Monitoring closely. Choosing alternatives when needed. If you’re taking isoniazid, don’t panic. But don’t ignore the signs. Your liver doesn’t scream until it’s too late. Stay alert. Stay informed. And talk to your doctor before you take anything else-especially over-the-counter painkillers.Can isoniazid cause permanent liver damage?
In most cases, no. About 95% of people who develop isoniazid-related liver injury recover fully after stopping the drug, usually within 4 to 8 weeks. Permanent damage is rare but possible if treatment continues despite severe symptoms like jaundice, confusion, or bleeding. Early detection and stopping the drug are critical to avoiding long-term harm.
Is it safe to take Tylenol (acetaminophen) while on isoniazid?
It’s not recommended. Both isoniazid and acetaminophen are processed by the same liver enzymes. Taking them together increases the risk of liver injury, even at normal doses. If you need pain relief, talk to your doctor about alternatives like acetaminophen-free options or very low doses with strict monitoring.
Do I need genetic testing before taking isoniazid?
Not routinely-but it helps if you’re at high risk. If you’re over 35, drink alcohol, have liver disease, or are of African or Asian descent (where slow acetylator rates are higher), asking for NAT2 testing could prevent serious liver damage. It’s standard in parts of Europe but not yet in the U.S. or most low-income countries due to cost and access.
How often should liver tests be done while on isoniazid?
Baseline testing is required before starting. For people with no symptoms, monthly liver function tests are recommended. If you have risk factors-like alcohol use, age over 35, or diabetes-your doctor may suggest testing every 2 weeks. If you develop any symptoms, get tested immediately, no matter when your last test was.
What are the alternatives to isoniazid for TB treatment?
For latent TB, rifampin alone for 4 months is an option. For active TB, newer regimens like the 4-month rifapentine-moxifloxacin combo or the 6-month BPaLM regimen (for drug-resistant TB) avoid isoniazid entirely. These are more expensive and not yet widely available everywhere, but they’re becoming the new standard in high-income countries.
Can I still take isoniazid if I have hepatitis B or C?
It’s risky. If you have chronic viral hepatitis, your liver is already under stress. Isoniazid can push it into failure. Doctors usually avoid it unless there’s no alternative. If used, it requires very close monitoring-often weekly liver tests-and sometimes lower doses. Many patients with hepatitis B or C are placed on alternative TB regimens to avoid the risk.






Samar Khan
OMG I took isoniazid for latent TB last year and my liver enzymes went through the roof 😭 I was just vibin’ thinking it was ‘just a pill’ but nooo… I ended up in the ER with jaundice. My doctor was like ‘you’re a slow acetylator’ and I had no idea what that even meant. Now I’m paranoid about every single supplement. Milk thistle? I’m taking it like it’s Gatorade now. 🍃
Nicole K.
You people are so irresponsible. If you’re gonna take drugs, you should do the research. No one forces you to take isoniazid. If you drink alcohol and don’t get tested, you’re asking for trouble. This isn’t rocket science. Stop blaming the medicine and take responsibility.
Amy Cannon
As someone who grew up in a household where herbal remedies were considered just as valid as pharmaceuticals, I find it fascinating how modern medicine is slowly catching up to what traditional cultures have known for centuries. Silymarin from milk thistle has been used in Ayurveda and Mediterranean folk medicine for liver detoxification for over 2,000 years. It’s not a miracle cure, but it’s a gentle, supportive ally - unlike the chemical hammer that is isoniazid. I’m not anti-science, I’m pro-wisdom. And yes, I did spell ‘silymarin’ right. Twice.
Himanshu Singh
Bro i was on isoniazid for 6 months and i didnt even know i was a slow acetylator till my mom forced me to get tested. Turned out i was. I started taking B6 like a champ and i felt way better. Also NO TYLENOL. I used ibuprofen and it was fine. Pls tell your friends. This info saved my liver 💪
Jasmine Yule
Thank you for writing this. Seriously. I’ve had three friends lose their liver function because they didn’t know about the risks. One of them is on the transplant list now. Please, if you’re reading this and you’re on isoniazid - get your enzymes checked. Talk to your doctor. Don’t wait until you’re yellow. I’m not mad, I’m just… heartbroken for you all. 🤍
Manan Pandya
It’s worth noting that the NAT2 polymorphism distribution correlates strongly with ancestral migration patterns. The high prevalence of slow acetylation in South Asia and sub-Saharan Africa is not a defect - it’s an evolutionary adaptation to environmental toxins. The real issue is the lack of culturally competent screening protocols in global health initiatives. Standardized protocols should include genetic risk stratification, especially in high-prevalence regions.
Aliza Efraimov
Okay I have to say - this is the most important thing I’ve read this year. I’m a nurse and I’ve seen too many patients get dismissed because ‘it’s just TB meds.’ One guy came in with encephalopathy because his ALT was over 2000 and everyone thought he was ‘just drunk.’ He wasn’t. He was on isoniazid. We need better education. Like, NOW. If you’re on this drug, get your liver checked every two weeks if you’re over 30 or drink anything with alcohol in it. I’m not joking. Your liver doesn’t text you back.
Emma Duquemin
Y’all are underestimating how wild this is. Isoniazid is basically a silent ninja assassin for your liver. One minute you’re fine, next minute you’re Googling ‘is jaundice contagious’ at 3 a.m. I took it for 9 months, did the B6, avoided alcohol, and still had a scary spike at month 7. My doctor said, ‘We’re stopping this.’ I cried. Not because I was mad - because I realized how little we’re told about what these drugs *really* do. I’m now on rifampin-only. No regrets. Also, milk thistle tea is delicious. I drink it with ginger. Life hack.
Kevin Lopez
Slow acetylators = high risk. NAT2 SNP rs1801280. CYP2E1 induction by rifampin = synergistic hepatotoxicity. Avoid acetaminophen. Monitor ALT/AST q4w. If >5x ULN, discontinue. Standard of care. No drama.
Duncan Careless
Just wanted to say I’m from the UK and we’ve been doing NAT2 testing for slow acetylators since 2018 in high-risk TB cases. It’s not perfect, but it’s better than waiting for someone to turn yellow. Also, no one talks about how hard it is to get milk thistle supplements approved in NHS pharmacies. Frustrating. But we’re trying.
Lisa Dore
Hey everyone - I’m a TB survivor. Took isoniazid for 9 months. Got the liver spike. Stopped. Got better. Now I help people navigate this stuff. If you’re scared, you’re not alone. I made a free Google Doc with all the resources, doctor questions to ask, and even a printable symptom tracker. DM me. I’ll send it. We’re in this together. 💙
Sharleen Luciano
It’s amusing how people treat isoniazid like it’s some mysterious poison. It’s a 70-year-old drug with well-documented risks. If you can’t handle basic pharmacokinetics, maybe you shouldn’t be taking it. The fact that we’re having this conversation at all suggests a systemic failure in patient education - not a flaw in the drug. Also, milk thistle? Really? That’s your solution? Cute.
Jim Rice
Actually, the 2016 study you cited had a tiny sample size. And the WHO’s new regimen? It’s only for drug-susceptible TB. What about MDR-TB? You’re oversimplifying. Also, ‘no alcohol’? I’ve been drinking wine with my TB meds for years. I’m fine. You’re all overreacting.