Every year, medication safety issues affect millions of people-not because they’re careless, but because the system is flawed. You take your pills as directed, trust your doctor, and assume the pharmacy got it right. But the numbers don’t lie: 1 in 20 patients worldwide suffer harm from medication errors. That’s not a rare accident. It’s a systemic problem-and you have more power to protect yourself than you think.
How Common Are Medication Errors?
Think about it: if you’re in a hospital, visiting a clinic, or just picking up a prescription at the pharmacy, you’re at risk. Globally, about 5% of patients experience avoidable harm from medications. That’s more than 130 million people a year. In the U.S. alone, over 1.5 million people are injured by medication errors annually. That’s more than the population of Wellington, New Zealand-every single year.
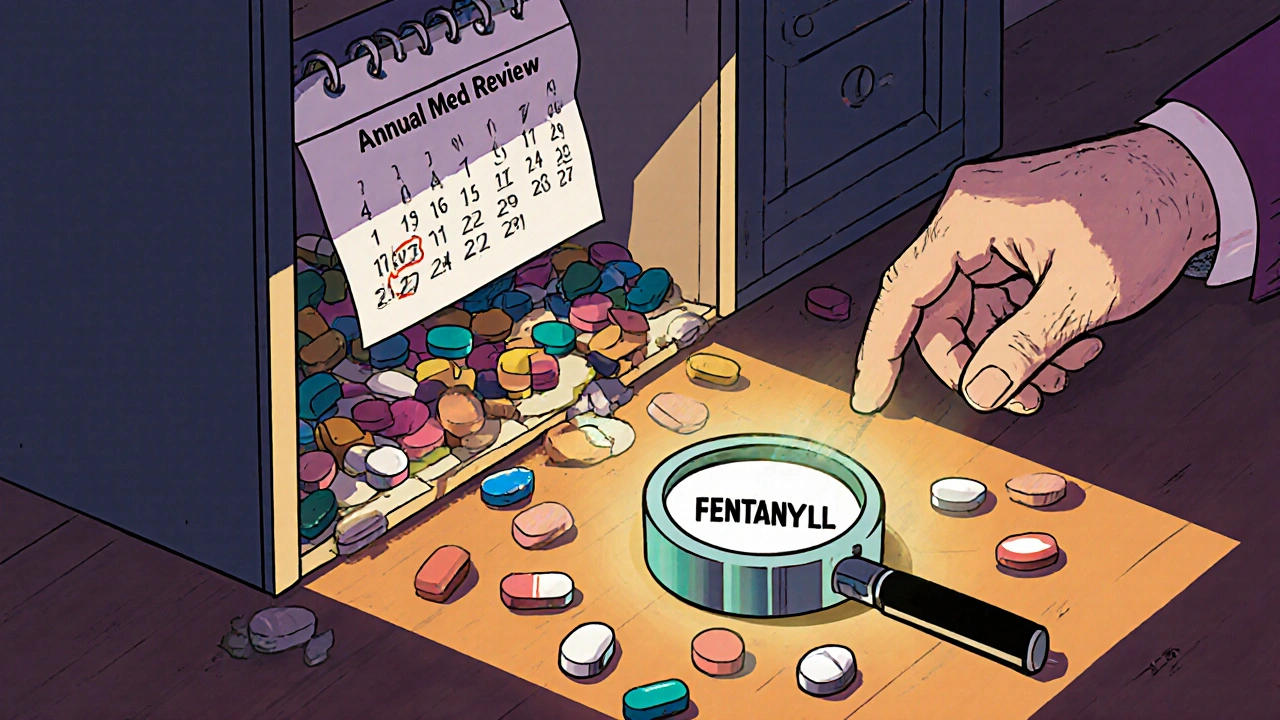
And it’s not just mistakes in dosing. A drug can be the right one, but given at the wrong time, mixed with another that shouldn’t be taken together, or even counterfeited. In 2023, the DEA seized over 80 million fake pills laced with fentanyl. Many of these were sold as oxycodone or Xanax but were actually deadly. One pill can kill.
Antibiotics, antipsychotics, and heart medications are the most common culprits behind serious harm. Why? Because they’re powerful. A small mistake in dosage can lead to organ failure, falls, confusion, or death. In hospitals, IV medications cause nearly half of all medication errors. At home, older adults are especially vulnerable-nearly 1 in 3 seniors take five or more medications daily, increasing the chance of dangerous interactions.
Who’s Most at Risk?
You might assume medication errors only happen in busy hospitals. But the truth is, most harm happens in your own home. Studies show between 2% and 33% of patients make mistakes with their meds at home. Common errors? Taking the wrong dose, skipping doses, mixing alcohol with pills, or not finishing a course because you “feel better.”
Older adults are the most affected group. In Australia, doctors cut antipsychotic prescriptions for seniors by 11% between 2016 and 2021-because those drugs often cause dizziness, falls, and even dementia-like symptoms in elderly patients. In the U.S., people over 65 account for nearly half of all hospital visits due to adverse drug events.
Younger people aren’t safe either. Nearly 9 million Americans misused prescription painkillers in 2021. Another 4 million used stimulants like Adderall without a prescription. Social media makes it easier than ever to buy pills from unregulated websites. Fentanyl is now the leading cause of death for Americans between 18 and 45.
Why Do These Errors Keep Happening?
It’s not because doctors or pharmacists are lazy. It’s because the system is overloaded. Nurses make errors between 16% and 44% of the time, depending on the hospital and workload. Pharmacists are rushing through hundreds of prescriptions a day. Electronic systems glitch. Handwritten notes get misread. And patients? They’re often too scared or too confused to ask questions.
Dr. Donald Berwick, a leading patient safety expert, put it simply: “Most medication errors are system failures, not individual failures.” That means blaming a nurse for giving the wrong pill misses the point. The real problem is poor communication, unclear labeling, lack of checks, and no clear process for patients to double-check their meds.
And then there’s the rise of counterfeit drugs. In North America, 1 in 3 fake drug seizures happen here. Pills bought online might look real, but they could contain rat poison, industrial chemicals, or lethal doses of fentanyl. The FDA’s own database recorded over 200,000 malfunction reports for infusion pumps between 2023 and 2024-including 204 deaths. These aren’t theoretical risks. They’re happening right now.
What’s Being Done to Fix This?
Some countries are making real progress. Australia launched 16 targeted actions to cut medication harm by 50% by 2025. They’ve already seen a 37% drop in opioid deaths since 2018 thanks to real-time prescription tracking. Hospitals now use barcode scanning to match the right drug to the right patient. Pharmacies are required to offer medication reviews for seniors.
In the U.S., Medicare is rolling out 16 new safety metrics for 2025. They’re tracking how often patients take their cholesterol, blood pressure, and diabetes meds correctly. They’re also monitoring high-dose opioid use and antipsychotic prescriptions in dementia patients. These aren’t just numbers-they’re life-or-death indicators.
Technology is helping too. AI tools are being tested to automatically check for drug interactions and flag risky prescriptions before they’re filled. One study predicts these tools could reduce errors by up to 30% by 2027. But tech alone won’t fix this. Patients need to be part of the solution.
What You Can Do Right Now to Stay Safe
You don’t need to be a medical expert to protect yourself. Here’s what works:
- Keep a current list of everything you take. Include prescription drugs, over-the-counter pills, vitamins, and supplements. Update it every time your doctor changes something.
- Use one pharmacy for all your prescriptions. That way, the pharmacist can spot dangerous interactions across all your meds.
- Ask three questions for every new prescription: What is this for? How and when do I take it? What side effects should I watch for? Don’t be shy-your life depends on it.
- Check your pills before you leave the pharmacy. If the color, shape, or label looks different from last time, ask why. Counterfeit pills are getting harder to spot, but inconsistencies are a red flag.
- Never buy meds online unless it’s a licensed pharmacy. Look for the VIPPS seal (Verified Internet Pharmacy Practice Sites). If it’s a website you found on Instagram or Facebook, don’t trust it.
- Review your meds with your doctor at least once a year. Especially if you’re over 65 or take five or more drugs. You might be taking something you no longer need.
Australia’s “5 Moments for Medication Safety” is a simple framework you can use: when you start a new drug, when you add one, when you’re discharged from the hospital, when you’re on a high-risk medication, and when you do a yearly review. Use these moments to ask questions, not just accept what’s given to you.

When Something Feels Wrong, Speak Up
One Reddit user shared that 68% of posts in r/meds were about confusion over dosage instructions. Another 22% were about side effects that weren’t explained. That’s not normal. If your doctor says, “This pill might make you dizzy,” but doesn’t say how long it’ll last or what to do if it gets worse-you need more info.
Don’t wait until you’re in the ER. If you feel off after starting a new medication, call your pharmacist. They’re trained to spot problems. If you’re unsure whether a symptom is normal, search the drug’s name + “side effects” on the FDA website. Don’t rely on Google ads or random blogs.
And if you think you’ve been given the wrong medicine? Say something. Show your pill bottle to the nurse, the doctor, the pharmacist. Say, “This doesn’t look right.” You have the right to know what you’re taking-and why.
The Bottom Line
Medication safety isn’t just about hospitals and regulations. It’s about you. You’re the last line of defense. No system is perfect. But when you know the risks, ask the questions, and stay informed, you cut your chances of harm in half.
Medication errors aren’t inevitable. They’re preventable. And you don’t need to wait for a policy change to make a difference. Start today: write down your meds. Call your pharmacy. Ask one question you’ve been too afraid to ask before. That one step could save your life-or someone you love’s.
How common are medication errors in the U.S.?
In the U.S., medication errors harm more than 1.5 million people each year, leading to about 7,000 deaths in hospitals alone. These errors include wrong doses, drug interactions, counterfeit pills, and miscommunication between providers.
What medications cause the most harm?
Antibiotics cause the highest number of medication-related harm events (about 20%), followed by antipsychotics (19%), central nervous system drugs (16%), and cardiovascular medications (15%). These drugs are powerful, and small mistakes can lead to serious or fatal outcomes.
Can I trust online pharmacies?
Only trust online pharmacies with the VIPPS seal (Verified Internet Pharmacy Practice Sites). Nearly 1 in 3 counterfeit drug seizures in the world happen in North America, and many fake pills sold online contain deadly doses of fentanyl. Never buy prescription drugs from social media ads or unverified websites.
What should I do if my pill looks different?
If your pill’s color, shape, size, or imprint changes without explanation, ask your pharmacist. It could be a generic version-but it could also be counterfeit. Always verify the medication before taking it, especially if you’re on high-risk drugs like opioids or anticoagulants.
Are seniors at higher risk for medication errors?
Yes. Older adults often take five or more medications daily, increasing the risk of harmful interactions. Antipsychotics, sedatives, and blood thinners are especially dangerous for seniors. Australia reduced inappropriate antipsychotic prescriptions for seniors by 11% between 2016 and 2021-showing that targeted reviews save lives.
What’s the biggest threat to medication safety today?
Fentanyl-laced counterfeit pills are the fastest-growing threat. In 2023, the DEA seized over 80 million fake tablets. These pills look real but can kill in minutes. They’re sold online and through social media, often marketed as oxycodone or Xanax. This is now the leading cause of death for Americans aged 18-45.






Corra Hathaway
Y’all seriously still trust pharmacies without double-checking? 😒 I had a pharmacist hand me a bottle of blue pills labeled 'oxycodone'-turned out to be fentanyl-laced crap. I called them out and they said 'it was a labeling error.' Like, wtf? I’m not dying for a typo.
Simone Wood
Let’s be real-this isn’t about patients being careless. It’s about corporate greed masquerading as healthcare. Pharmacies are underpaid, nurses are overworked, and Big Pharma is flooding the market with counterfeit generics while lobbying against regulation. The system is designed to fail you. And now they want us to ‘ask three questions’ like that’s some magical shield against death-by-pill? 🤡
Clifford Temple
Why are we even talking about this like it’s a surprise? America’s healthcare system is a dumpster fire wrapped in a lawsuit. I’ve seen nurses give the wrong med because they were doing 12 shifts a week. Pharmacists miss interactions because they’re scanning 200 scripts an hour. And now you want grandma to ‘review her meds annually’? She can’t even remember her own name half the time. This isn’t empowerment-it’s negligence dressed up as advice.
Florian Moser
Actually, the advice in this post is spot-on. Keeping a med list, using one pharmacy, asking questions-these aren’t just tips, they’re survival tactics. I’m a nurse, and I’ve watched patients die because they didn’t speak up. It’s not about blaming the system-it’s about using the tools we have. If you’re scared to ask, write it down first. Say it out loud. Your life isn’t a gamble.
Paula Jane Butterfield
As someone who immigrated here from a country where meds are sold over the counter like candy, I can tell you-this system is terrifying. But the advice here? Gold. I made my mom keep a color-coded spreadsheet of everything she takes. Even her vitamins. She thought I was crazy. Then she had a fall because she mixed her blood thinner with a new supplement. Now she’s the one reminding me to check labels. Small steps save lives. 🙏
Swati Jain
Y’all are missing the point. This isn’t just about pills-it’s about power. Who gets to decide what you take? A doctor who spends 7 minutes with you? A pharmacist who’s never met you? A bot that flags interactions but doesn’t know you’re vegan and take turmeric daily? Tech isn’t fixing this. People are. Ask. Challenge. Document. Don’t let them gaslight you into silence. And if you’re on Adderall because your boss says ‘perform or quit’? Yeah, that’s part of this too.
jim cerqua
Let me tell you about my cousin. 27. Healthy. Took a ‘Xanax’ from a guy at a party. Died in 12 minutes. The pill had fentanyl. The guy? Got 18 months. The system? Still selling fake pills on Instagram. This isn’t a ‘statistic.’ This is genocide. And they’re calling it ‘drug abuse’ while the real killers? They’re on the board of some pharma company drinking champagne. #FentanylIsAMurderWeapon
Donald Frantz
Interesting that the post mentions AI reducing errors by 30% by 2027 but doesn’t mention liability. If an algorithm approves a lethal interaction and someone dies, who’s responsible? The coder? The hospital? The FDA? We’re automating risk without accountability. And if you think ‘checking labels’ is enough-you’re ignoring how sophisticated counterfeits have become. Some pills now have FDA-approved-looking imprint codes. You can’t visually verify anymore. We need mandatory blockchain tracking. Not just ‘ask questions.’
Shawn Sakura
hey everyone i just wanted to say this post really made me think. i used to think i was fine taking my meds however i wanted but after reading this i started writing everything down and using one pharmacy. my dr was shocked i knew my own med list. i even asked about my blood pressure med-turns out i was on the wrong dose. i feel so much better now. its not hard, just take 5 minutes. you got this. 💪