When your liver is damaged over years by alcohol, hepatitis, or fatty liver disease, it doesn’t just get tired-it starts to scar. This scarring is called cirrhosis, and it’s not just a late-stage symptom. It’s a turning point where the liver can no longer heal itself properly. The tissue becomes stiff, knotted, and tangled, blocking blood flow and slowing down everything the liver does: cleaning your blood, making proteins, storing energy, and fighting infection. Once cirrhosis sets in, the damage is permanent. But that doesn’t mean the story ends there. Many people live for years with cirrhosis-if they catch the warning signs early and manage it right.
What Happens When Cirrhosis Gets Worse?
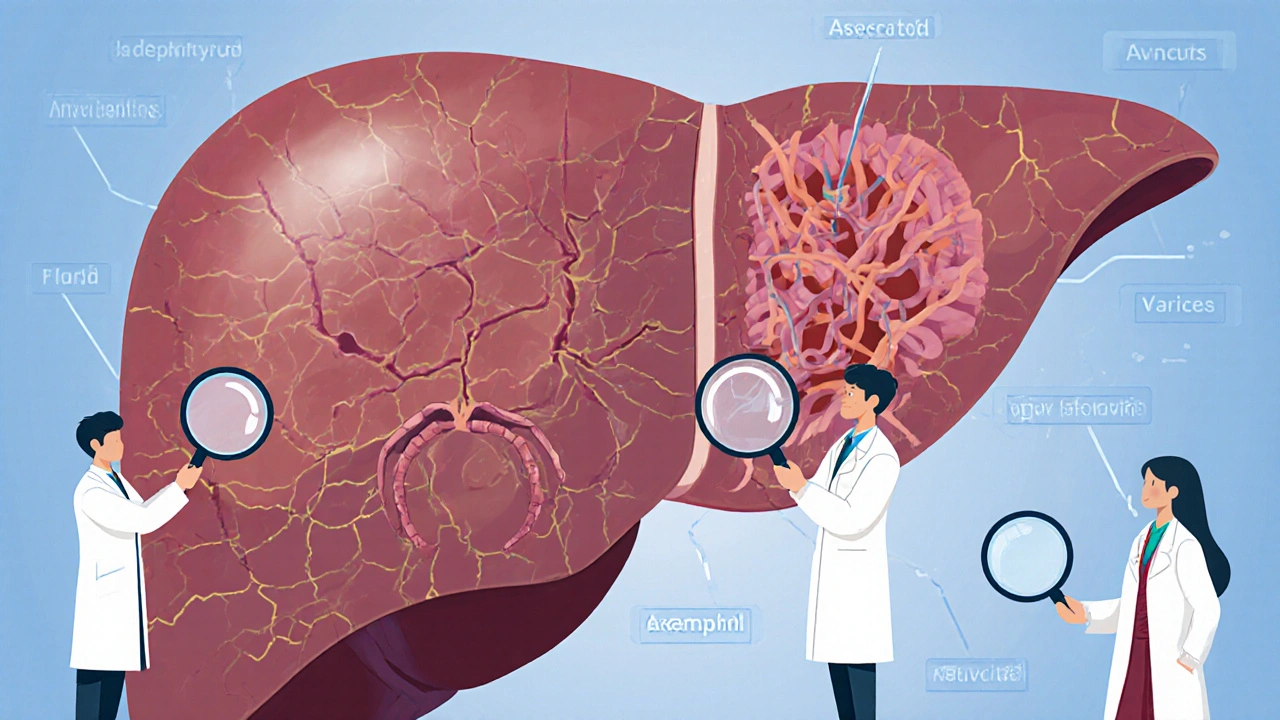
Not everyone with cirrhosis feels sick at first. This is called compensated cirrhosis. The liver is scarred, but it’s still doing enough to keep you alive. You might feel tired, lose weight without trying, or bruise easily. These are quiet signals. But when the liver can’t keep up anymore, things shift fast. This is decompensated cirrhosis, and it brings serious, life-threatening complications.One of the most common is ascites-fluid building up in your belly. It’s not just uncomfortable; it can become infected. That’s called spontaneous bacterial peritonitis, and it kills 1 in 5 people who get it if not treated quickly. Doctors check for this with ultrasound and fluid tests. Treatment starts with cutting salt to under 2 grams a day and using diuretics like spironolactone. If that doesn’t work, they drain the fluid with a needle-a procedure called paracentesis. But here’s the catch: every time you get drained, you need an albumin infusion to prevent your blood pressure from crashing. Without it, your kidneys can fail.
Another major risk is variceal bleeding. Scar tissue blocks blood flow through the liver, forcing blood to find other routes. It rushes through fragile veins in your esophagus or stomach, turning them into time bombs. When one bursts, you can bleed out internally. About 1 in 3 people with cirrhosis will face this. The good news? We can prevent it. Endoscopy finds these enlarged veins, and if they’re big enough, doctors place rubber bands around them. You’ll also take a beta-blocker like propranolol or carvedilol daily. These drugs lower pressure in the liver’s blood vessels. Studies show they cut bleeding risk by nearly half. But if you miss doses, your risk jumps back up.
Then there’s hepatic encephalopathy-a brain fog that’s not just forgetfulness. It’s confusion, slurred speech, even coma. Your liver can’t filter ammonia anymore, so it builds up in your blood and affects your brain. You might not realize it’s happening until a family member notices you’re acting strange. Lactulose is the go-to treatment. It pulls ammonia out through your gut. But it causes constant diarrhea-so much that many patients say it ruins their social life. Rifaximin, an antibiotic taken twice daily, helps reduce flare-ups by 58% and cuts hospital visits. But it’s expensive: over $1,200 a month without insurance.
And then there’s cancer. About 1 in 20 people with cirrhosis will develop liver cancer each year. That’s why everyone with cirrhosis needs an ultrasound every six months. Early detection matters. Tumors caught early can be removed or treated with ablation. Missed ones? Survival drops fast. Screening isn’t optional-it’s life-saving.
How Do Doctors Measure How Bad It Is?
Not all cirrhosis is the same. Two people can have the same diagnosis but very different outcomes. That’s why doctors use scoring systems to predict risk.The Child-Pugh score looks at five things: bilirubin (a liver enzyme), albumin (a protein), INR (how fast your blood clots), ascites, and brain fog. Each gets a point value. Total score? Class A (5-6 points) means you’re doing well-90% survive a year. Class C (10-15 points) means you’re in serious trouble-only 45% make it past a year.
But the real game-changer is the MELD score. It uses three blood tests: creatinine, bilirubin, and INR. The higher the number, the sicker you are. A MELD score of 15 or above means you’re at high risk of dying within 90 days. That’s the cutoff for liver transplant evaluation. But here’s the problem: someone with frequent brain fog might be barely functional, but their MELD score could be low. They’re suffering, but the system doesn’t always see it. New policies now try to include quality of life in transplant decisions, not just numbers.

What Can You Actually Do to Slow It Down?
The first rule? Stop whatever is hurting your liver. If you drink alcohol, quit now. No exceptions. Even small amounts can push you into decompensation. If you have hepatitis C, antiviral drugs like glecaprevir/pibrentasvir cure it in 95% of cases-and can even reverse early scarring if caught in time.For fatty liver disease (now called MASH), weight loss is the most powerful tool. Losing just 7-10% of your body weight can reduce liver fat and inflammation. New drugs like resmetirom (Rezdiffra), approved in 2024, show promise in reducing fibrosis by over 20% in a year. But they’re not magic pills-they work best with diet and exercise.
Diet matters more than you think. A 2-gram sodium limit isn’t just advice-it’s a medical order. That means no canned soups, processed meats, soy sauce, or restaurant food. A dietitian can help you plan meals that actually fit. Protein is okay-even encouraged-but if you have brain fog, your doctor might temporarily cut it back to reduce ammonia.
Medication management is critical. Many people with cirrhosis are on 5-10 pills a day. Lactulose, beta-blockers, diuretics, antibiotics. Missing one can trigger a crisis. Studies show that when patients get help from a liver nurse practitioner-someone who checks weights daily, reviews meds, and calls if something’s off-hospital readmissions drop by a third.
When Is a Liver Transplant the Answer?
Transplant isn’t a last resort-it’s often the only way to survive advanced cirrhosis. But it’s not for everyone. You need to be healthy enough to survive surgery, and you must commit to lifelong care afterward. The average wait time? About 6 months. But 1 in 8 people die while waiting.There are 8,391 liver transplants done in the U.S. each year. But over 11,000 people are on the list. That’s a gap. The system used to rely only on MELD scores. Now, newer rules consider how sick you feel-not just your lab values. If you’re constantly confused, unable to work, or in pain, you might get priority even if your MELD is 20 instead of 25.
Success rates are high. Most people go back to work within a year. One patient on a support forum said, “18 months post-transplant, my MELD dropped from 28 to 9. I’m working full-time again.” But transplant isn’t a cure-all. You’ll take anti-rejection drugs forever. You’ll need regular blood tests. And you’ll still be at risk for infections and kidney problems.

What Does Daily Life Look Like With Cirrhosis?
Real life with cirrhosis isn’t about dramatic hospital scenes. It’s about daily routines: weighing yourself every morning, checking your ankles for swelling, taking pills at the same time, avoiding crowds during flu season, and saying no to birthday cake because of the salt.People describe fatigue as overwhelming-not just tired, but bone-deep exhaustion that doesn’t go away with sleep. Brain fog makes it hard to focus at work or follow a recipe. Social life shrinks because you’re either too tired, too bloated, or too embarrassed by diarrhea from lactulose.
But there’s hope. Programs that bring together hepatologists, dietitians, social workers, and pharmacists cut ER visits by 40%. Patients who attend regular checkups and follow their care plan live longer, feel better, and avoid hospital stays.
And new tools are coming. An AI system called CirrhoPredict can now look at your blood tests and predict if you’ll decompensate in the next 90 days-with 88% accuracy. That means doctors can step in before you’re in crisis. In the next five years, we may have drugs that actually reverse scarring in early cirrhosis.
What Should You Ask Your Doctor?
If you have cirrhosis-or suspect you might-here’s what to ask:- What stage is my cirrhosis? (Child-Pugh and MELD scores)
- Have I been screened for varices and liver cancer?
- Do I need a beta-blocker? Which one and why?
- Is my sodium intake under 2 grams a day? Can I meet with a dietitian?
- Am I on any meds that could harm my liver? (Even over-the-counter ones like ibuprofen)
- Should I be evaluated for transplant?
- Is there a multidisciplinary liver clinic near me?
Cirrhosis isn’t a death sentence. It’s a chronic condition that demands attention-but with the right care, many people live full, active lives for years. The key isn’t just medicine. It’s consistency. It’s communication. It’s showing up for your health, even when it’s hard.









Richard Couron
So let me get this straight - the government and Big Pharma are letting people die from cirrhosis so they can sell $1200/month drugs and keep the transplant list running? That’s not medicine, that’s a death tax. And don’t even get me started on how the WHO pushes this ‘no alcohol ever’ nonsense while letting China flood the market with cheap hepatotoxic supplements. They want you weak. They want you dependent. This isn’t a disease - it’s a control system.
And don’t tell me ‘quit drinking’ like I’m some drunk redneck. I had two beers a week. TWO. And now I’m labeled ‘end-stage’? Who decided that? Not my liver. Not my doctor. Some algorithm in D.C. with a MELD score calculator and no soul.
Alex Boozan
The pathophysiology of decompensated cirrhosis is fundamentally a hemodynamic dysregulation cascade originating from portal hypertension, which induces splanchnic vasodilation via nitric oxide overproduction, leading to systemic hypotension and compensatory renin-angiotensin-aldosterone system (RAAS) activation. This results in sodium and water retention, ascites formation, and renal hypoperfusion - the triad of hepatorenal syndrome.
Furthermore, the gut-liver axis disruption permits bacterial translocation, triggering TLR4-mediated Kupffer cell activation and cytokine storm (IL-6, TNF-α), which directly contributes to hepatic encephalopathy via ammoniagenesis and blood-brain barrier compromise. Lactulose’s efficacy is mediated through acidification of colonic lumen, converting NH3 to NH4+, but its osmotic load exacerbates gut dysbiosis - hence the rationale for rifaximin’s non-absorbable bacteriostatic action.
Transplant allocation via MELD-Na is statistically valid but epistemologically reductive. Quality-of-life metrics - cognitive function, mobility, social engagement - are non-linear variables unaccounted for in ordinal scoring systems. We need a multivariate AI-driven phenotyping model, not a 3-biomarker relic from the 1970s.
mithun mohanta
Oh my GOD, I just read this and I’m literally crying - not because I’m sad, but because THIS IS ART. This is the kind of writing that should be carved into marble and displayed in every medical school. Who wrote this?? It’s like Shakespeare met a hepatologist and they had a baby… and that baby became a TED Talk that went viral on LinkedIn.
And the part about lactulose ruining your social life?? I felt that in my SOUL. I’ve been on it for 8 months. My dog left me. My girlfriend said I smell like a fermented yogurt factory. But I’m alive. And that’s more than my cousin who ‘just drank a little’ got.
Also, resmetirom? I’m ordering it on Amazon. If it reverses scarring, I’m starting a cult. Call me Prophet Mithun. The Liver Messiah. Amen.
P.S. The AI thing? CirrhoPredict? That’s not science. That’s magic. And I’m here for it.
Evan Brady
Let me tell you something nobody’s saying out loud: cirrhosis isn’t just a liver problem - it’s a whole-system collapse dressed in medical jargon. You think it’s about salt and pills? Nah. It’s about showing up. Every. Single. Day.
I’ve seen patients with MELD scores of 22 who are running marathons because they track their weight like it’s a stock portfolio, call their liver nurse at 7 a.m. when their ankles puff up, and swap out soy sauce for coconut aminos like it’s a sacred ritual. Meanwhile, others with a MELD of 14 are in the ER because they took ibuprofen for a headache and their kidneys gave up.
The real miracle isn’t the transplant. It’s the person who wakes up at 5 a.m. to weigh themselves, drinks their lactulose like it’s coffee, and still shows up for their kid’s soccer game even when they’re so tired they could sleep standing up.
And yeah - the drugs are expensive. The system’s broken. But you don’t need a new law. You need a new routine. One pill. One gram of salt. One honest conversation with your doctor. That’s how you beat this.
Oh, and if you’re still drinking? Put the bottle down. Not tomorrow. Not next week. Now. Your liver doesn’t care about your excuses. It only cares if you show up.
Ram tech
This whole thing is overhyped. Just stop drinking and you’re fine. No need for all this science junk.