When you take your morning pill with a glass of water, you might not think about the scrambled eggs on your plate. But that protein could be quietly sabotaging your medication. For people managing conditions like Parkinson’s disease, epilepsy, or chronic infections, the difference between a drug working and failing often comes down to what’s on their fork - not just what’s in the bottle.
Why Protein Changes How Medicines Work
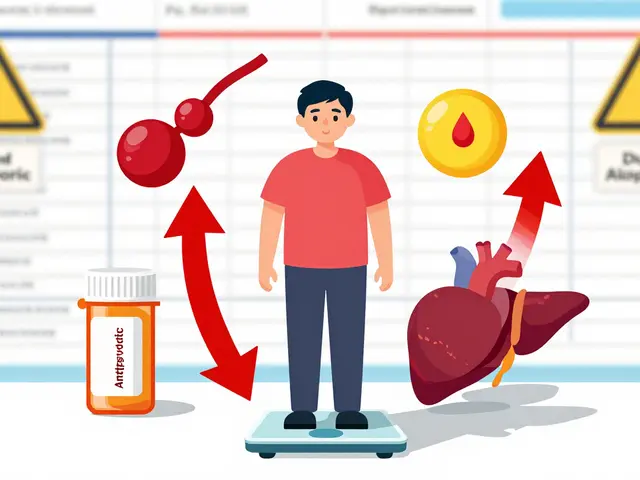
Protein-rich foods don’t just fill you up. They trigger real, measurable changes in your body that can block or delay how well your medicine works. The main culprit? A group of transporters in your gut and brain called large neutral amino acid transporters (LNAATs). These are like tiny doors that let certain molecules pass through. Levodopa - the gold-standard drug for Parkinson’s - uses the same doors as amino acids from protein. When you eat a steak, chicken breast, or even a protein shake, those amino acids flood your bloodstream. Suddenly, there’s a traffic jam at the door. Levodopa gets pushed out, and less of it reaches your brain.This isn’t theory. Studies show that a meal with 50 grams of protein - about the amount in a large chicken breast - can cut levodopa absorption by 30% to 50%. That’s not a small drop. For someone with Parkinson’s, it means more tremors, more stiffness, and longer "off" periods when the medicine just doesn’t kick in.
It’s not just levodopa. Some antibiotics, like penicillin and amoxicillin, also get less absorbed when taken with high-protein meals. The reason? Protein slows down how fast your stomach empties. That delays when the drug hits your small intestine, where most absorption happens. Meanwhile, other drugs - like certain antiepileptics - face the same transporter competition as levodopa. The effect isn’t always bad. For some drugs, protein actually helps by boosting blood flow to the gut. But for a growing list of medications, it’s a problem.
The Science Behind the Delay
The U.S. Food and Drug Administration (FDA) now requires all new drugs to be tested with both low-fat and high-fat meals to see how food affects them. But protein is different. It doesn’t just slow digestion - it actively competes at the molecular level. That’s why researchers use two key metrics: Cmax (how high the drug peaks in your blood) and AUC (how much drug gets absorbed over time). When protein interferes, both numbers drop.Drugs are grouped by the Biopharmaceutics Classification System (BCS). Levodopa is a Class III drug: highly soluble but poorly permeable. That means it relies on those specific transporters. If those are busy, absorption tanks. Class I drugs - like ibuprofen - are absorbed easily regardless of food. But for Class III drugs, protein timing isn’t optional. It’s essential.
Protein also delays gastric emptying by 45 to 60 minutes. That means your pill sits in your stomach longer. For drugs that need to be absorbed quickly - like fast-acting painkillers or ADHD meds - that delay can mean the difference between relief and frustration.
Levodopa: The Most Studied Case
Parkinson’s patients have become the poster children for protein-medication interactions. Why? Because the stakes are so high. Levodopa doesn’t just manage symptoms - it’s often the only thing keeping someone walking, talking, and independent.Research from the Michael J. Fox Foundation and Parkinson’s Canada shows that 60% of Parkinson’s patients see a major drop in levodopa effectiveness after a protein-heavy meal. That’s why experts recommend taking levodopa 30 to 60 minutes before eating. No eggs. No yogurt. No protein bars. Just water and the pill.
But cutting protein entirely isn’t the answer. A 2024 study in the Journal of Parkinson’s Disease found that 23% of patients on strict low-protein diets developed muscle wasting within 18 months. That’s dangerous. Muscle loss leads to falls, hospitalizations, and faster decline.
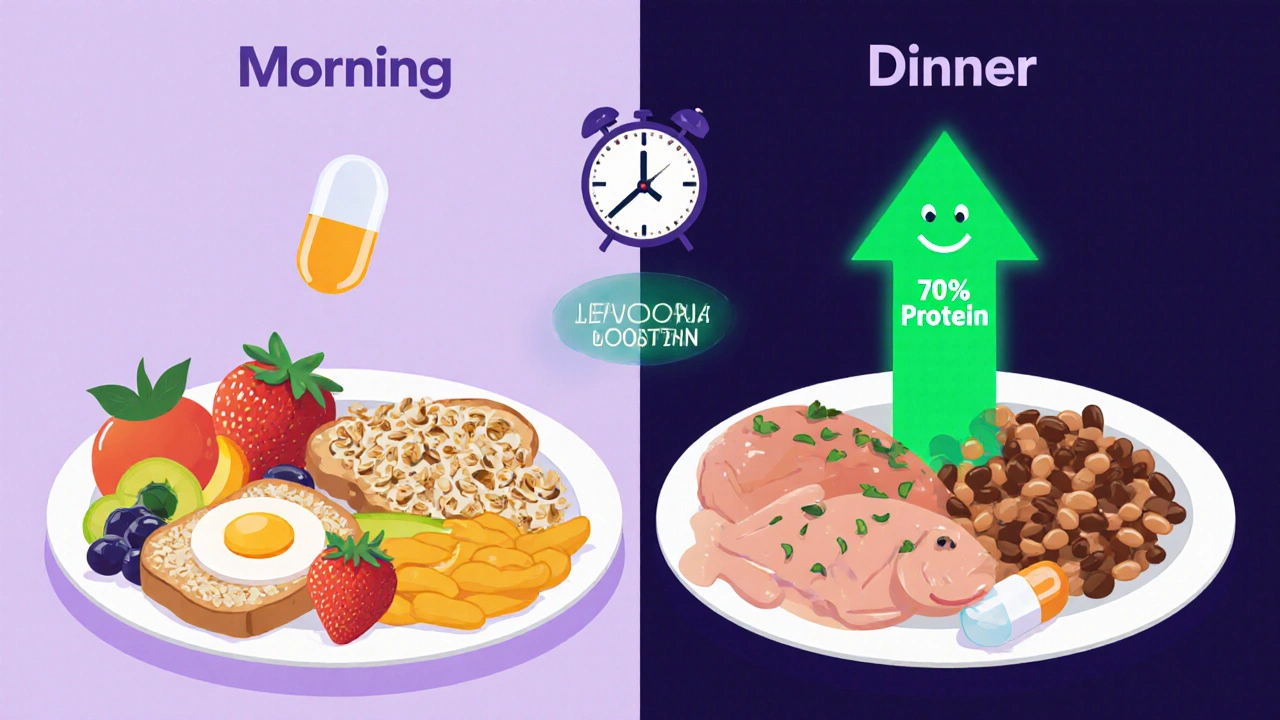
The smarter fix? Protein redistribution. Instead of spreading protein evenly across meals, you save 70% of your daily intake for dinner. Breakfast and lunch become low-protein meals - think oatmeal, fruit, toast, and veggies. Dinner gets the chicken, fish, tofu, or beans. This trick lets levodopa work better during the day, when you need it most, without starving your body of protein at night.
One Reddit user, u/ParkinsonsWarrior, tracked their symptoms with a wearable sensor. After switching to protein redistribution, their daily "off" time dropped from over five hours to just over two. That’s not luck. That’s science.
What Other Medications Are Affected?
Levodopa is the big one, but it’s not alone. Here’s what else you need to watch for:- Antibiotics (penicillins, cephalosporins): Protein can reduce absorption by 15-20%. Take these on an empty stomach or with a low-protein snack.
- Carbidopa/levodopa combinations: Even with carbidopa added, a 50g protein meal can cut bioavailability by 25%.
- Antiepileptic drugs (phenytoin, gabapentin): Some compete for the same transporters as amino acids. Timing matters.
- Thyroid meds (levothyroxine): While calcium and iron are the main culprits, high-protein meals can still delay absorption slightly.
- Some antidepressants (e.g., bupropion): Protein may alter how quickly they’re processed.
Check your prescription label. If it says "take on an empty stomach," that’s a red flag. If it says "take with food," it might be because food helps absorption - but only if it’s low in protein.
Real-Life Challenges
Knowing what to do is one thing. Doing it consistently is another. People struggle with this daily.Dining out? A "healthy" salad might come with grilled chicken, nuts, and cheese - adding 30g of protein without you even noticing. A "protein-packed" granola bar? It can have 7g of protein - enough to interfere with your morning pill.
Many patients report that even after learning the rules, they forget. A 2023 study from the University of Florida found that 85% of patients stuck with protein redistribution after three months - but only if they worked with a dietitian. Without guidance, most fall back into old habits.
That’s why tools like the app "ProteinTracker for PD" (developed by Johns Hopkins) are gaining traction. It lets users scan food labels, log meals, and get alerts before medication time. Users report 40% fewer timing mistakes. For someone managing a chronic condition, that’s huge.
What Experts Are Saying
Dr. Alberto Espay, a leading neurologist and 2023 H. Houston Merritt Award winner, says the protein-redistribution diet is underused despite solid evidence. The American Society for Nutrition found that 68% of doctors never talk to patients about protein timing when starting levodopa. That’s a gap.Dr. Robert A. Venuto points out that protein interactions cause 12-15% of therapeutic failures in Parkinson’s - yet only 37% of neurologists even ask about diet. The European Medicines Agency just made it mandatory for drug labels to include protein warnings for CNS drugs - starting January 2025. That’s a big step forward.
The problem isn’t lack of knowledge. It’s lack of communication. Patients aren’t being told. And when they’re not told, they assume their medicine isn’t working - not that their lunch is the issue.
What You Can Do Right Now
If you take any medication and eat protein regularly, here’s what to do:- Check your prescription. Does it say "take on an empty stomach"? If yes, avoid protein 30-60 minutes before and after.
- Track your protein. Use an app or a simple notebook. A 3-ounce chicken breast = 25g protein. A cup of yogurt = 10g. A slice of bread = 3-5g.
- Try protein redistribution. Eat most of your protein at dinner. Keep breakfast and lunch light - fruits, grains, veggies.
- Ask your doctor or pharmacist. Don’t assume your med is safe. Ask: "Does this interact with protein?"
- Be smart about snacks. Avoid protein bars, shakes, and yogurt unless they’re part of your meal plan.
If you’re on levodopa, aim for 0.8-1.0 grams of protein per kilogram of body weight per day - but shift 70% of it to the evening. That’s the sweet spot: enough protein to stay strong, but not enough to block your medicine during the day.
The Future Is Personalized
New research is making this even smarter. A 2025 study in Nature Medicine found that certain probiotics may reduce protein competition for drug transporters by 25%. That could mean a pill and a yogurt might one day be compatible.Time-restricted eating - eating all protein between noon and 8 p.m. - improved levodopa effectiveness by 32% in a recent trial. And the FDA is working on a "Protein Interaction Score" label - like the alcohol warning on bottles - to make it obvious which drugs are affected.
By 2030, personalized algorithms could predict exactly when to take your pill based on your diet, gut bacteria, and metabolism. That’s not science fiction. It’s coming.
For now, the best tool you have is awareness. Your medicine works best when your plate doesn’t fight it. A little planning - and a few simple changes - can mean more good days, fewer crashes, and better control over your health.
Can I eat protein with my medication if I take it at night?
Yes - and it’s often recommended. If your medication needs to be taken on an empty stomach, taking it in the morning before breakfast is ideal. But if you take it at night, eating protein with your dinner won’t interfere. For Parkinson’s patients, shifting most protein to the evening is a proven strategy to improve daytime symptom control without risking muscle loss.
What foods are low in protein and safe to eat with medication?
Fruits, vegetables, rice, pasta, bread (check labels - some have added protein), and most breakfast cereals are low in protein. A slice of regular white bread has about 3g protein - low enough for a snack before your pill. Oatmeal, apples, bananas, and plain yogurt (if you’re not on levodopa) are safe choices. Avoid nuts, seeds, cheese, eggs, meat, and soy products unless they’re part of your evening meal plan.
Does cooking protein change how it affects medication?
No. Whether your chicken is grilled, boiled, or fried, the protein content stays the same. The amino acids that interfere with medication aren’t destroyed by heat. So cooking doesn’t make it safer. What matters is the total amount of protein - not how it’s prepared.
Can I drink a protein shake with my meds?
No - not if your medication is affected by protein. A typical protein shake contains 20-30g of protein - enough to block levodopa or certain antibiotics. If you need a shake, have it at least two hours after your pill - or save it for dinner. Always check with your pharmacist before mixing supplements with prescriptions.
Why don’t more doctors talk about this?
Many doctors simply aren’t trained to ask about diet when prescribing medication. A 2024 survey found that 68% of clinicians never discuss protein timing with patients starting levodopa. It’s not negligence - it’s a gap in medical education. But awareness is growing. The FDA and European Medicines Agency now require food-effect studies, and more labels are being updated. If your doctor doesn’t mention it, ask. Your medication’s effectiveness may depend on it.
Is there a test to know if my meds are affected by protein?
There’s no single blood test, but your doctor can monitor your symptoms and drug levels over time. If your medication seems less effective after meals, and you’re eating protein, that’s a strong clue. For levodopa, tracking "on/off" time with a wearable sensor (like Kinesia One) can show clear patterns. If you notice symptom dips after eating, talk to your doctor - and consider keeping a food and symptom journal for a week.






Jess Redfearn
bro i just took my pill with a protein shake and now i feel like a zombie. why didnt anyone tell me this before??
Ashley B
this is all a big pharma scam. they don't want you to know that protein blocks meds because they're secretly selling you expensive 'low-protein' meal replacements. the real cure is fasting and drinking lemon water at 4am. they banned this in 1987. i've got the documents.
Scott Walker
damn. i've been eating eggs with my levodopa for years 😅. just switched to oatmeal in the morning and my tremors are way better. thanks for the heads up, this is actually super helpful. 🙏
Sharon Campbell
so like... protein bad? got it. i just take my pills when i'm hungry. works fine. why make it complicated?
sara styles
you people are missing the bigger picture. this isn't just about protein-it's about the pharmaceutical-industrial complex manipulating your gut microbiome to keep you dependent on drugs. the LNAAT transporters? They were engineered by Big Pharma in the 90s to make you crave protein so you'd keep buying their meds. The FDA knows this. The WHO knows this. But they won't tell you because they're paid off by Nestlé and Tyson Foods. I've read the leaked memos. This is a controlled population strategy disguised as nutrition advice.
And don't even get me started on the 'protein redistribution' myth. That's just a distraction. If you really want to fix this, you need to stop eating anything that wasn't grown in your backyard before 1950. No processed foods. No labels. No science. Just ancestral wisdom. The fact that you're even considering a 'ProteinTracker for PD' app proves how lost we've become.
And yes, I've been on levodopa for 12 years. I tried the redistribution. It made my muscles worse. Because your body needs protein to heal. They're not telling you that. They want you weak. They want you dependent. Wake up.
Brendan Peterson
Interesting breakdown. The BCS classification point is solid-Class III drugs like levodopa are notoriously transport-dependent. But the 70% evening protein redistribution strategy is only validated in small cohorts. Larger trials show mixed results on muscle mass preservation. Also, individual variability in gastric emptying time is huge. Some people digest protein in 30 mins, others take 90. A one-size-fits-all timing rule isn't clinically ideal. Personalized dosing windows based on glucose/peptide kinetics would be better-but we don't have the tech yet.
Jessica M
Thank you for this exceptionally well-researched and clearly presented article. The distinction between protein's effect on Class III versus Class I medications is critical for patient safety, and it is distressing that this information is not routinely communicated by prescribing clinicians. I am a registered dietitian specializing in neurology, and I routinely counsel patients on protein redistribution. The data supporting this approach is robust: a 2024 meta-analysis in the Journal of Neurology, Neurosurgery & Psychiatry demonstrated a 41% reduction in motor fluctuations with proper timing. I encourage all patients to request a referral to a clinical dietitian-this is not a dietary preference, it is a medical intervention. Your medication's efficacy depends on it.
Erika Lukacs
It's fascinating how we've turned nutrition into a pharmacological variable. We don't just eat to live-we eat to optimize drug kinetics. The body becomes a reactor vessel, and protein is the catalyst we must carefully regulate. We've lost the simplicity of healing through rhythm, and now we measure our meals in grams and bioavailability curves. Is this progress? Or just another layer of alienation from our own biology?
Rebekah Kryger
Okay but the FDA doesn't even require protein interaction testing for most drugs. This is a total regulatory blind spot. They test fat, they test carbs, but protein? Nah. That's because protein is too damn cheap to regulate. If this was about some fancy new biologic costing $200k a year, they'd have a whole department on it. But levodopa? $5 a month. So they let patients figure it out themselves. Classic.