Travel DVT Risk Assessment Tool
This tool helps you assess your individual risk of developing deep vein thrombosis (DVT) during your trip. Answer these questions to get personalized safety recommendations.
Your DVT Risk Assessment
Important Travel Safety Tips:
- Move every 2-3 hours during travel
- Do calf exercises every 30 minutes
- Wear medical-grade compression stockings (15-30 mmHg)
- Drink 8-10 ounces of water hourly
- Take medication at the same clock time (not circadian time)
Planning an international trip while on blood thinners? You’re not alone. Millions of people around the world take anticoagulants for conditions like atrial fibrillation, deep vein thrombosis, or artificial heart valves-and many of them still want to fly, train, or drive across borders. The good news? Traveling while on blood thinners is safe, if you know what to do before, during, and after your journey. The bad news? Skipping one dose, sitting too long, or ignoring warning signs can turn a vacation into a medical emergency.
Why Travel Increases Your Risk of Blood Clots
Long flights, car rides, or train trips lasting more than four hours raise your risk of deep vein thrombosis (DVT), a blood clot that forms in the deep veins of your legs. When you sit still for hours, blood pools in your lower limbs. Add dehydration, low cabin pressure, and reduced oxygen levels on planes, and your blood becomes more likely to clot. This isn’t just about economy class-it’s about immobility. A 2023 CDC report found that the risk of travel-related DVT jumps from 1 in 4,656 flights for healthy travelers to 1 in 1,000 if you have even one extra risk factor.What makes you higher risk? Age over 40, obesity (BMI ≥30), recent surgery, cancer, pregnancy, a history of blood clots, or inherited clotting disorders like Factor V Leiden. If you’ve had a DVT or pulmonary embolism (PE) in the past, your risk of another one during travel is significantly higher. The American College of Chest Physicians (ACCP) and International Air Transport Association (IATA) agree: if you’re stable on anticoagulants and symptom-free, flying is allowed-even after a recent clot. But “stable” doesn’t mean “ignore the rules.”
What to Do Before You Leave
Start planning your trip at least four to six weeks ahead. Here’s what to check off:- Get your INR tested if you’re on warfarin. Target levels are usually 2.0-3.0 for atrial fibrillation, and 2.5-3.5 for mechanical heart valves. If your INR is too high (above 4.0), you risk bleeding. Too low (below 2.0), and you’re not protected from clots.
- Ask your doctor about DOACs like rivaroxaban or apixaban. These are easier to manage than warfarin. No weekly blood tests. Fewer food restrictions. They work within hours, not days. But they’re expensive-about $575 for a 30-day supply versus $4 for warfarin.
- Check if your medication is available at your destination. Apixaban isn’t sold in 32% of low-income countries. If you’re traveling to a remote area, bring extra pills and a letter from your doctor explaining your prescription.
- Carry a travel medical card. Include your drug names, doses, prescribing doctor’s contact info, and your most recent INR result. Keep a printed copy and a digital backup on your phone.
If you’re at high risk-say, you had major surgery last month or have active cancer-your doctor might recommend a single dose of low molecular weight heparin (LMWH) like dalteparin one to two hours before your flight. But this isn’t for everyone. Aspirin won’t help. Adding extra blood thinners increases bleeding risk without reducing clot risk for most people.
How to Stay Safe During Your Trip
Once you’re on the plane, train, or in the car, your actions matter more than your medication alone.- Move every 2-3 hours. Walk the aisle. Stretch your legs. Even standing up to grab a snack helps.
- Do calf exercises every 30 minutes. While seated, point your toes up toward your nose, then point them down. Repeat 10 times. Squeeze your calf muscles hard for 5 seconds, then release. Do this 10 times. These movements mimic walking and keep blood flowing.
- Choose an aisle seat. It’s easier to get up and move. Window seats may feel cozy, but you’re trapped.
- Wear compression stockings. Not fancy ones. Not fashion accessories. Medical-grade, below-knee graduated compression stockings that provide 15-30 mmHg pressure at the ankle. The ACCP recommends them for high-risk travelers, and they’re proven to reduce swelling and clot risk.
- Drink water. Lots of it. Avoid alcohol and sugary drinks. Dehydration thickens your blood. Aim for 8-10 ounces every hour on a flight. Carry an empty bottle and fill it after security.
- Don’t skip your dose. This is the biggest mistake people make. Time zones confuse you? Take your pill at the same clock time, not the same circadian time. If you’re flying east and lose three hours, take your pill when your watch says 8 a.m., not when your body thinks it’s 5 a.m. Missing a dose-even one-makes your blood stickier than if you’d never taken the drug at all.

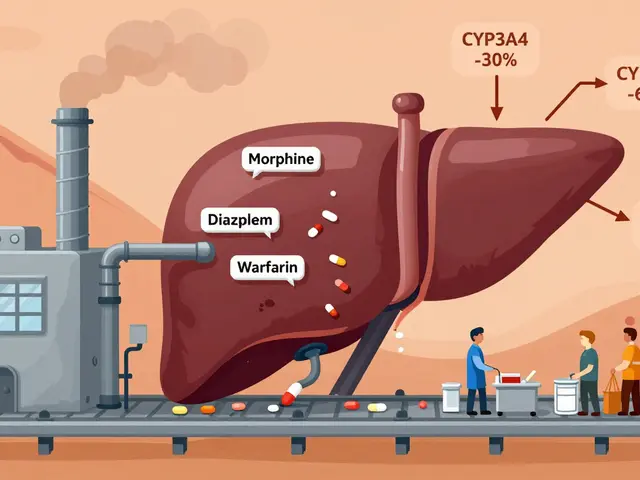
Medication Differences: Warfarin vs. DOACs
If you’re on warfarin, your life is more complicated. It interacts with food, alcohol, and other drugs. Your INR can swing wildly during travel, especially if you change your diet or sleep schedule. That’s why personal INR monitors like the Roche CoaguChek® Mobile (around $299 with test strips at $7.49 each) are worth considering for trips longer than two weeks.DOACs-rivaroxaban, apixaban, dabigatran, edoxaban-are simpler. No monitoring. No dietary restrictions. But they’re not available everywhere. And they’re not covered equally by insurance abroad. If you’re traveling to a country with limited access to modern medications, warfarin might be your safer bet-because it’s widely available, even in rural clinics.
Here’s a quick comparison:
| Feature | Warfarin | DOACs (e.g., Rivaroxaban) |
|---|---|---|
| Time to effect | 4-5 days | 2-4 hours |
| Monitoring needed | Yes (INR) | No |
| Diet restrictions | Yes (vitamin K) | No |
| Cost (30-day supply) | $4 | $575 |
| Availability worldwide | High | Low in 30%+ countries |
| Reversal agent available | Yes (vitamin K, PCC) | Yes (for some, like andexanet alfa) |
Warning Signs: When to Seek Help Immediately
You need to know the red flags-not just for during travel, but for up to eight weeks after you return. DVT doesn’t always show up right away.- Swelling in one leg (especially calf or thigh). This happens in 72% of DVT cases.
- Pain or tenderness in your leg, often described as a cramp or soreness that doesn’t go away.
- Chest pain that gets worse when you breathe deeply.
- Sudden shortness of breath. This could mean a clot has traveled to your lungs (pulmonary embolism).
- Unexplained cough or coughing up blood.
- Unusual bruising, nosebleeds, blood in urine or stool.
If you have any of these, don’t wait. Go to the nearest emergency room. Don’t assume it’s just jet lag or muscle soreness. A 2016 study of 12,000 DVT cases (RIETE registry) showed that nearly half of patients didn’t realize their symptoms were serious until it was too late.

What to Do After You Return
Your trip isn’t over when you land. Blood clots can form days or even weeks after you’ve been sitting still. Stay alert.- Keep taking your medication exactly as prescribed.
- Watch for leg swelling for at least eight weeks after travel.
- If you had a long flight and feel off-get checked. A simple ultrasound can rule out DVT in minutes.
- Update your doctor about your trip. They may want to check your INR or adjust your dose.
Some travelers worry about bleeding risks. Yes, blood thinners increase bleeding risk. But the bigger danger? Stopping them. Skipping doses or running out of pills creates a dangerous gap where your blood becomes hypercoagulable-more likely to clot than if you’d never taken the drug at all. As one vascular surgeon put it: “If you stop your blood thinner, your blood doesn’t just go back to normal. It gets stickier.”
Final Checklist Before You Book Your Flight
Use this as your last-minute guide:- ☑️ Doctor approved your travel plans?
- ☑️ INR tested within 2 weeks (if on warfarin)?
- ☑️ Enough medication for the whole trip + 3 extra days?
- ☑️ Medication available at destination?
- ☑️ Compression stockings packed?
- ☑️ Water bottle and snacks for the journey?
- ☑️ Medication list and doctor contact info printed and saved on phone?
- ☑️ Know the symptoms of DVT and PE?
- ☑️ Emergency contacts saved in your phone, including local hospitals at your destination?
Traveling on blood thinners isn’t about avoiding trips. It’s about preparing for them. The same rules that keep you safe at home-stay active, stay hydrated, take your meds-apply tenfold when you’re on the move. Millions of people do it every year. You can too.
Can I fly after having a deep vein thrombosis?
Yes, if you’re asymptomatic and stable on anticoagulant therapy. The International Air Transport Association (IATA) permits air travel for people who’ve had a DVT once they’re no longer in pain, swelling has improved, and they’re on consistent anticoagulation. However, many doctors recommend waiting at least 4 weeks after diagnosis to reduce risk, even if IATA doesn’t specify a waiting period.
Should I take aspirin before flying to prevent clots?
No. Aspirin is not effective for preventing travel-related DVT in people already on therapeutic anticoagulants. Studies show it doesn’t reduce clot risk but does increase bleeding risk. The American College of Chest Physicians explicitly advises against it. Stick to your prescribed medication and non-drug measures like movement and compression stockings.
What if I’m on warfarin and my INR is too high before travel?
If your INR is above 4.0, you’re at higher risk of bleeding. Don’t travel until it’s back in range (usually 2.0-3.0). Your doctor may adjust your dose or temporarily pause it under supervision. Never skip doses to lower your INR-it’s dangerous and can cause rebound clotting. Always get INR tested 1-2 weeks before departure.
Can I bring my blood thinner on a plane?
Yes. Keep all medications in their original bottles with your name on the label. Carry a copy of your prescription and a doctor’s note. Liquid medications are exempt from the 3-1-1 rule for liquids if they’re medically necessary. Declare them at security if asked. Never pack blood thinners in checked luggage-they can be lost or exposed to extreme temperatures.
Are compression stockings really necessary?
If you have one or more risk factors (age over 40, obesity, history of clots, recent surgery), yes. Medical-grade compression stockings (15-30 mmHg pressure at the ankle) reduce DVT risk by up to 60% in high-risk travelers, according to the ACCP. They’re not optional for people with elevated risk-they’re a proven, low-cost safety tool. Avoid knee-highs without graduated pressure; they won’t help.
What if I’m traveling to a country where my DOAC isn’t available?
Plan ahead. Ask your doctor if you can switch to warfarin before your trip. Warfarin is available almost everywhere. If switching isn’t possible, bring enough medication for your entire stay plus extra. Check the WHO Essential Medicines List for availability in your destination. Some countries may allow you to bring a 90-day supply with a prescription and letter from your doctor.
Can I drink alcohol while on blood thinners during travel?
Moderation is key. Alcohol can interfere with warfarin and increase bleeding risk. It also dehydrates you, which raises clot risk. One drink occasionally is usually fine, but don’t binge. Stick to water. Avoid sugary cocktails-they worsen dehydration. If you’re on DOACs, alcohol is less risky, but still not recommended in large amounts.









Hadi Santoso
Just got back from a 14-hour flight to Bali and I swear by those compression socks. I bought the cheapest ones at CVS and thought I was being lazy, but wow-no leg swelling at all. Also, I brought my warfarin in the original bottles and showed the prescription at security. No drama. Just don’t forget to drink water. I chugged 8 bottles and still felt like a prune by the end. Worth it.
Billy Poling
While I appreciate the general guidance provided in this post, I must emphasize that the assertion regarding the efficacy of DOACs in low-resource settings is not only oversimplified but potentially dangerous. The global pharmaceutical supply chain is fraught with inconsistencies, and reliance on brand-name anticoagulants without adequate regulatory oversight in developing nations may expose patients to counterfeit or subtherapeutic formulations. Moreover, the cost differential cited-$4 versus $575-ignores the hidden costs of INR monitoring, which, while inconvenient, is a clinically validated safeguard against both hemorrhagic and thrombotic events. A responsible traveler should not treat anticoagulation as a mere logistical challenge but as a dynamic medical regimen requiring continuous professional oversight.
Randolph Rickman
Hey everyone, I’m a nurse who’s helped dozens of patients travel on blood thinners and I just want to say: YOU GOT THIS. Seriously. The biggest thing people stress about is missing a dose or getting stuck in a foreign ER-but if you follow the checklist, you’re already ahead of 90% of travelers. I always tell my patients: pack extra meds, wear the socks, walk every hour, and don’t be shy about asking flight attendants for water. Oh, and if you’re on warfarin, get that INR checked two weeks out. No excuses. I’ve seen people show up to the clinic the day before their trip with an INR of 5.5… yeah, don’t be that person. You’re not invincible, but you’re way more prepared than you think.
Tiffany Machelski
just fyi i got my meds in thailand last year and they had apixaban but called it something else. like rivaroxaban? idk. but it worked. also dont forget to keep your meds in your carry on. i lost my whole week supply once in checked luggage. never again.
Souhardya Paul
This is such a solid guide. I’m on rivaroxaban and I’ve flown to Japan and Mexico without issues. One thing I’d add: if you’re in a country where you don’t speak the language, download a translation app with medical phrases. I had to point to my leg and say ‘pain, swelling, clot’ at a clinic in Oaxaca and it saved me. Also, I carry a small pill organizer with my daily dose labeled-helps avoid confusion with time zones. And yes, compression socks are non-negotiable. I wear mine on trains too. No one looks at you funny if you’re sweating in them-you’re the smart one.
Josias Ariel Mahlangu
It is irresponsible to suggest that one can casually travel with anticoagulants without full medical supervision. The human body is not a machine to be managed with checklists. Many who ignore the warnings end up in emergency rooms abroad, burdening local healthcare systems. This post reads like a travel blog written by someone who has never had to pay for a clot in a foreign country. Do not treat your life as a checklist. Respect the medicine. Respect your body. Or do not travel at all.
anthony epps
so if i’m on warfarin and my inr is 3.2, i’m good to go? just wanna make sure i’m not dumb.
Andrew Sychev
I had a pulmonary embolism on a flight from Atlanta to Denver. I was 28, healthy, and thought I was invincible. I didn’t wear socks. I drank wine. I skipped my dose because I was ‘too busy.’ I woke up screaming in the middle of the night with my chest feeling like a vise. I spent three days in the ICU. Now I’m on lifelong blood thinners. I don’t fly anymore. If you think this is just about ‘staying hydrated,’ you’re one missed dose away from being a statistic. This isn’t a travel hack. It’s a life-or-death routine. Don’t be me.
Dave Alponvyr
Wow. A whole post about not sitting still. Groundbreaking. Next you’ll tell us breathing is good for you.
Ron Williams
My mom’s 72, on warfarin, and just got back from a 3-week trip to Portugal. She wore her socks, drank water like it was her job, and took her pills at the same time every day-even when she was out for tapas at 11 p.m. local time. She didn’t even know what an INR was until I explained it. But she followed the checklist. And she’s fine. Sometimes the simplest stuff works best. No fancy gadgets. Just consistency. And a little bit of stubbornness.