Drug Formulary: What It Is, How It Works, and What You Need to Know
When your doctor prescribes a medication, the first question your pharmacist might ask isn’t about dosage—it’s about your drug formulary, a list of medications approved for coverage by a health plan or hospital system. Also known as a medication formulary, it determines what drugs you can get at a lower cost—or sometimes, if you can get them at all. This isn’t just paperwork. It directly impacts whether you’ll pay $5 or $500 for your pills each month.
Every health plan, from Medicare Part D to private insurers, builds its own drug formulary, a curated list of medications chosen based on cost, safety, and clinical effectiveness. These lists aren’t random. They’re shaped by negotiations between insurers and drugmakers, and often favor generics or older drugs that have proven track records. But here’s the catch: if your drug isn’t on the list, you might need prior authorization, step therapy, or even a full appeal just to get it covered. That’s why understanding your formulary isn’t optional—it’s essential for managing costs and avoiding treatment gaps.
Formularies don’t just affect what you take—they shape how you take it. For example, if your insulin isn’t on formulary, you might be pushed toward a cheaper alternative that doesn’t work as well for you. Or if you’re on a long-term medication like levothyroxine, a formulary change could force you to switch brands, even if your body reacts poorly to the new version. The same applies to asthma inhalers like Foracort or diabetes combos like Actoplus Met. These aren’t just names on a list—they’re part of your daily health routine.
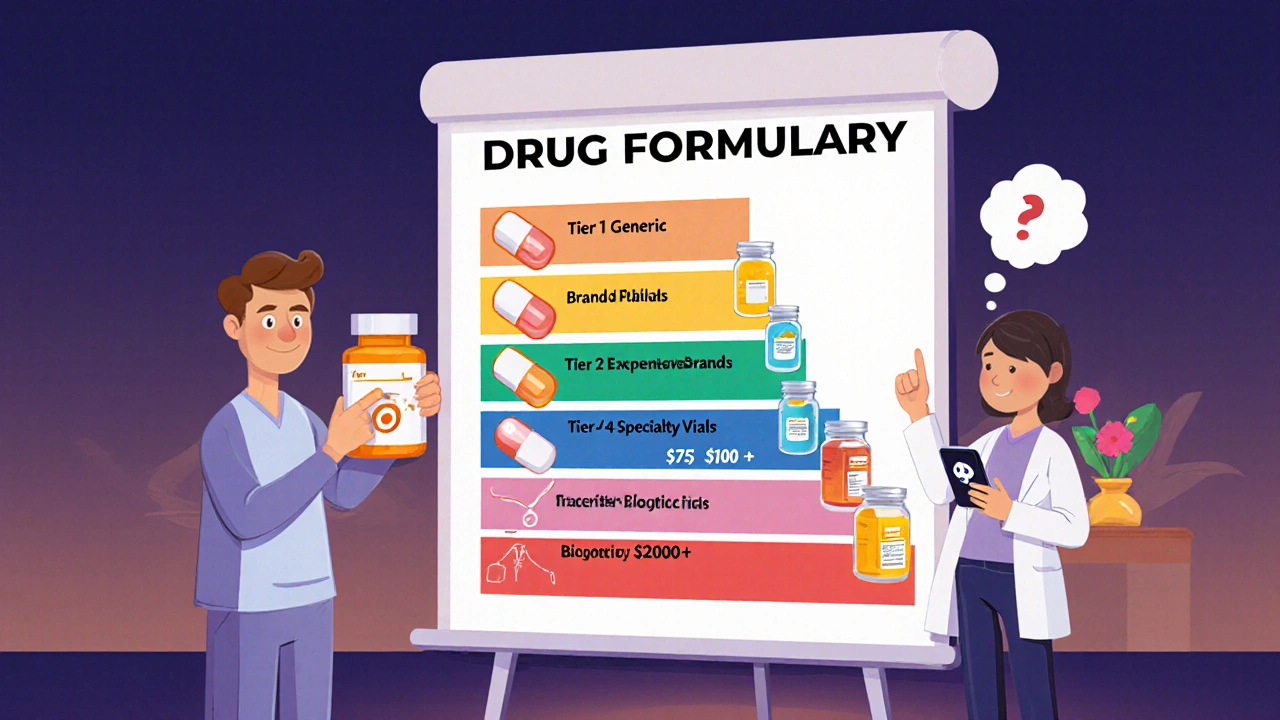
Some formularies include tiers—Tier 1 for generics, Tier 4 for specialty drugs—and each tier comes with different out-of-pocket costs. You might not realize that a drug you’ve been taking for years suddenly moved from Tier 2 to Tier 3, and your copay jumped from $15 to $75. That’s why checking your formulary every year during open enrollment matters. It’s not just about new drugs—it’s about protecting what you already rely on.
And it’s not just insurers. Hospitals and clinics have their own internal pharmacy formulary, a restricted list of drugs approved for use within their facility. If you’re admitted and your home medication isn’t on their list, they’ll substitute it—sometimes with something less effective or with different side effects. That’s why bringing a full list of your meds to the hospital isn’t just smart—it’s a safety must.
Drug shortages? Formularies shift fast. When insulin or azithromycin runs short, formularies get updated overnight to include alternatives. That’s how you end up on a different antibiotic or a new diabetes pill without warning. Knowing how formularies work helps you ask the right questions: Is this substitution safe? Is there a generic? Can I appeal this decision?
The posts below dive into real-world cases where formulary decisions made or broke treatment. From how SGLT-2 inhibitors got flagged for rare infections to why levothyroxine interactions with calcium can ruin your thyroid control, these stories show how formulary rules ripple through your health. You’ll find guides on finding alternatives during shortages, spotting hidden formulary traps, and talking to your pharmacist like a pro. This isn’t theory—it’s what happens when insurance lists meet your medicine cabinet.
A drug formulary is your insurance plan's list of covered medications. Learn how tiers, exceptions, and new 2025 rules affect your out-of-pocket costs and how to find the best coverage for your prescriptions.