When you have type 2 diabetes, losing weight isn’t just about fitting into smaller clothes-it’s one of the most powerful tools you have to take back control of your health. Many people think diabetes means you’re stuck with high blood sugar forever, but the truth is, weight loss can reverse it. Not always completely, but often enough to cut medications, reduce heart risks, and feel like yourself again.
Why Weight Loss Matters for Diabetes
Extra fat, especially around the belly, doesn’t just sit there. It sends signals that make your body resistant to insulin-the hormone that moves sugar from your blood into your cells. When insulin doesn’t work well, sugar builds up. That’s type 2 diabetes. But when you lose even a small amount of weight-5% to 7% of your body weight-your cells start responding to insulin again. Your pancreas doesn’t have to work as hard. Your blood sugar drops. And you might not need as many pills or insulin shots.
The Diabetes Prevention Program (DPP), a major U.S. study from the early 2000s, showed that people with prediabetes who lost 5-7% of their body weight cut their risk of developing full-blown diabetes by 58%. That’s more than double the effect of the drug metformin. Fast forward to today, and the same principles apply. The American Diabetes Association now says weight loss isn’t just helpful-it’s a core part of treatment.
How Much Weight Should You Aim to Lose?
You don’t need to lose 50 pounds to see results. Losing just 10 to 15 pounds can make a huge difference. For someone who weighs 200 pounds, that’s only 5-7.5% of body weight. Studies show that losing this much leads to:
- A drop in A1C levels by 0.5% to 1.0%
- Lower blood pressure and triglycerides
- Less need for diabetes medications
- Improved energy and mobility
And in some cases-especially if you’ve had diabetes for less than six years-losing 10-15 kg (22-33 lbs) can lead to remission. That means your blood sugar stays in the normal range without any medication. The DiRECT trial in the UK proved this: nearly half of participants who lost around 10 kg went into remission after one year.
What Works: The Most Effective Strategies
Not all diets or workouts are created equal when you have diabetes. Here’s what the science says actually works.
1. Eat Less, But Eat Smarter
Creating a daily calorie deficit of 500-750 calories is the sweet spot for steady, safe weight loss-about 1 to 1.5 pounds per week. But how you cut calories matters.
Focus on:
- High-fiber carbs: vegetables, beans, lentils, oats, and whole grains. Aim for at least 14 grams of fiber per 1,000 calories you eat.
- Lean protein: chicken, fish, tofu, eggs, Greek yogurt. Protein keeps you full longer and helps preserve muscle as you lose fat.
- Healthy fats: avocado, nuts, olive oil. These don’t spike blood sugar.
- Portion control: Use smaller plates, measure servings, and avoid eating straight from packages.
The Mediterranean diet has shown strong results in diabetes management. It’s not a fad-it’s simple: more plants, less processed food, olive oil instead of butter, fish instead of red meat. In the DiRECT trial, people following a low-calorie Mediterranean-style plan lost an average of 10 kg and had nearly a 50% remission rate.
2. Move More-But Not Just Walking
Walking is great, but it’s not enough on its own. The CDC recommends at least 150 minutes of moderate activity per week-like brisk walking, cycling, or swimming. But you also need strength training.
Why? Muscle burns more calories than fat, even at rest. Strength training two or three times a week improves insulin sensitivity more than cardio alone. Try bodyweight exercises like squats, lunges, push-ups, or use resistance bands. You don’t need a gym. A 20-minute session at home, twice a week, makes a real difference.
3. Use Technology to Stay on Track
People who use apps to track food, activity, and blood sugar lose more weight than those who don’t. Apps like MyFitnessPal, MySugr, or Glucose Buddy help you spot patterns. Did your sugar spike after lunch? Maybe it was the rice. Did you feel better after a weekend hike? That’s your motivation.
Telehealth coaching also works. The CDC’s National Diabetes Prevention Program offers online sessions with certified coaches. In 2024, over 200,000 people enrolled in Medicare’s version of this program-and 65% completed the full course. Those who stuck with it lost an average of 8% of their body weight.
4. Medications That Help You Lose Weight
Some diabetes meds cause weight gain-like insulin and sulfonylureas. Others help you lose it. If you’re struggling, talk to your doctor about switching.
- GLP-1 agonists (like semaglutide/Wegovy or liraglutide): These reduce appetite and slow digestion. People lose an average of 15% of their body weight over a year.
- SGLT2 inhibitors (like empagliflozin or dapagliflozin): These make your kidneys flush out extra sugar through urine. You lose 2-5 pounds and lower your heart risk.
- Tirzepatide (Mounjaro): Approved in 2023 for weight loss, this newer drug combines GLP-1 and GIP actions. In trials, people lost nearly 21% of their body weight.
These aren’t magic pills. They work best with diet and exercise. And they can cause nausea or stomach upset at first-start low, go slow.
What Doesn’t Work (and Why)
There’s a lot of noise out there. Fad diets, juice cleanses, keto without medical supervision-these often backfire.
- Very low-carb diets can work for some, but they’re hard to sustain. If you’re on insulin or sulfonylureas, going too low-carb can cause dangerous lows. Always adjust meds with your doctor first.
- Extreme calorie restriction (under 1,000 calories/day) slows your metabolism, makes you tired, and can cause muscle loss. That makes it harder to keep weight off.
- Skipping meals leads to blood sugar swings and overeating later.
- Weight loss pills from the internet are unregulated and risky. Some contain hidden stimulants that can raise your heart rate or blood pressure.
The goal isn’t speed-it’s sustainability. Losing weight slowly means your body adapts. Your habits stick. And your blood sugar stays stable.
Real People, Real Results
On the American Diabetes Association’s community forum, one user wrote: “I lost 22 pounds in six months. Walked 150 minutes a week. Measured my food. My A1C dropped from 7.2% to 5.9%. I cut my metformin in half.”
Another on Reddit said: “I hit a plateau at 3 months. Then I started lifting weights twice a week. Lost another 18 pounds in four months. My energy? Sky-high.”
But it’s not all smooth sailing. Some people struggle with emotional eating. Others can’t tolerate GLP-1 meds because of nausea. A 2023 survey found that 42% of people with diabetes said stress or emotions were their biggest barrier to losing weight.
That’s why support matters. Join a group. Talk to a coach. Find a buddy. Celebrate non-scale wins: better sleep, climbing stairs without getting winded, not needing to check your sugar as often.
What to Watch Out For
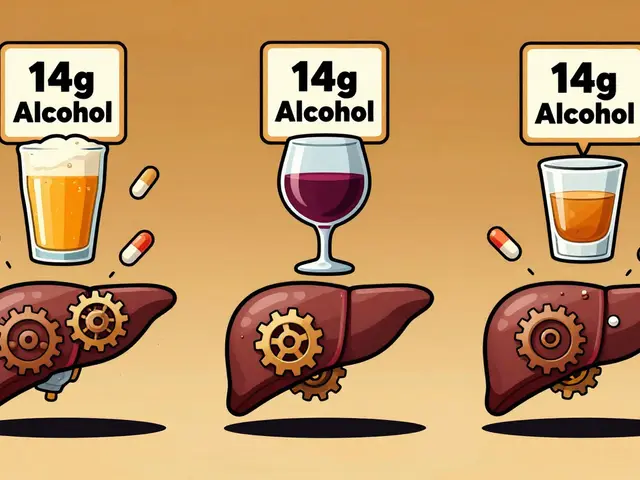
Weight loss can be risky if you’re on certain meds. If you’re taking insulin or sulfonylureas, losing weight too fast can cause low blood sugar. That’s dangerous.
Here’s what to do:
- Check your blood sugar more often when you start losing weight.
- Talk to your doctor before making big changes. They may lower your insulin dose or switch you to a weight-neutral med.
- If you feel shaky, sweaty, or dizzy, treat it like a low-even if your meter says it’s normal. Your body might be adjusting.
Older adults need extra care. Losing weight too fast can increase fracture risk. Focus on preserving muscle, not just dropping pounds. Strength training is even more critical here.

How to Keep It Off
Most people lose weight. Fewer keep it off. The Look AHEAD trial found that only 27% maintained a 10% weight loss after four years. Why? Life happens. Stress. Holidays. Work. Kids.
Long-term success means building habits, not following plans. Here’s how:
- Keep weighing yourself weekly. It’s not about perfection-it’s awareness.
- Plan meals ahead. Cook in batches. Have healthy snacks ready.
- Make movement part of your day: take the stairs, walk during calls, park farther away.
- Reconnect with your why. Was it to play with your grandkids? To stop taking five pills a day?
- Don’t wait for motivation. Do it anyway. Action builds motivation.
And remember: if you gain a few pounds back, don’t give up. Just reset. One bad week doesn’t erase six months of progress.
Where to Get Help
You don’t have to do this alone.
- Ask your doctor for a referral to a certified diabetes care and education specialist (CDCES). These professionals help you create a personalized plan. People who work with them lose 2.3 times more weight than those who don’t.
- Check if your insurance covers the National Diabetes Prevention Program (NDPP). It’s a year-long program with weekly group coaching. Many Medicare and private plans cover it for free.
- Use free tools: the CDC’s website has meal plans, activity trackers, and videos. The American Diabetes Association’s Food Hub offers portion-controlled recipes.
Technology is helping too. Apps that sync with your glucose monitor now give real-time feedback: “Your sugar rose after this meal-try swapping white rice for quinoa next time.” It’s like having a coach in your pocket.
And if you’re ready for more-there are now clinical programs that combine weight loss, continuous glucose monitoring, and AI-driven coaching. These are still emerging, but they’re the future.
The Bottom Line
Diabetes and weight loss aren’t separate battles-they’re the same fight. You don’t need to be perfect. You don’t need to lose 100 pounds. You just need to lose 5-7% of your body weight and keep it off. That’s enough to lower your A1C, reduce your meds, and feel stronger every day.
Start small. One change at a time. Walk 10 minutes after dinner. Swap soda for sparkling water. Measure your rice. Talk to your doctor about your meds. Build from there.
This isn’t about willpower. It’s about strategy. And with the right plan, you can take your health back-no matter how long you’ve had diabetes.





Kaylee Crosby
Just wanted to say this post hit different. I lost 18 lbs in 5 months using the Mediterranean plan + twice-weekly bodyweight workouts. My A1C dropped from 7.8 to 5.7 and I haven't touched metformin in 4 months. You don't need to be perfect, just consistent. One step at a time 💪
Mariam Kamish
Yeah right. They always say 'lose 5-7%' like it's easy. Meanwhile my insurance won't cover GLP-1s and my job makes me work 12-hour shifts. This is just rich people advice wrapped in science-speak 😒
Adesokan Ayodeji
As someone from Nigeria who's helped over 30 people manage diabetes through diet changes, I can tell you the real game-changer is community. In my village, we cook together, walk after sunset, and share meals without guilt. No apps needed. Just people holding each other accountable. The science backs it, but the heart makes it stick. 🌍❤️
Lawrence Zawahri
They don't want you to know this but Big Pharma paid the ADA to push weight loss as the 'solution' so they can sell you more drugs later. GLP-1s cost $1k/month. They don't care if you're healthy, they care if you're hooked. The real cure? Stop eating their processed poison. That's not in the article because it doesn't make money 🤫
Patrick Goodall
WEIGHT LOSS IS A LIE. The real problem is insulin resistance caused by glyphosate in our food supply. They don't tell you the FDA approved it because Monsanto owns them. I lost 30lbs on keto but my sugar stayed high until I switched to organic grass-fed everything. Now I'm cured. No meds. No science. Just truth. 🌱💣
Karen Ryan
I'm a Filipina-American who grew up eating white rice daily. I didn't believe I could change until I found a local church group that cooked healthy Filipino meals together. We swapped rice for cauliflower rice, used coconut oil instead of lard, and walked after Sunday service. It wasn't about restriction-it was about reconnection. I lost 12 lbs and my mom finally stopped worrying. 🙏
Dirk Bradley
While the empirical data presented is statistically significant, one must interrogate the epistemological foundations of the DiRECT trial. The reliance on self-reported dietary intake introduces significant measurement error, and the exclusion criteria disproportionately eliminate low-income populations. The recommendation of calorie deficits without addressing structural determinants of health constitutes a neoliberal fallacy. One cannot 'lose weight' when food deserts and wage stagnation dictate dietary options. 📊
Benjamin Gundermann
Look, I get it. You wanna feel better. But let’s be real-nobody’s gonna lose weight just because some article says so. I tried all this stuff. Walked, tracked, ate kale, drank water. Felt like crap. Then I started lifting. Not much. Just 20 mins twice a week. Now I feel like I’m 30 again. No magic. Just showing up. You don’t need to be perfect. Just show up. That’s it. 🤝
Emma Hanna
HOW DARE YOU suggest that weight loss can 'reverse' diabetes?! This is dangerous misinformation! Diabetes is a genetic condition! You can't 'fix' it by eating less! This is the same dangerous rhetoric that blames victims for their illness! Shame on you for promoting this! 😡
Rachelle Baxter
Wow. This is so irresponsible. You're telling people to just 'swap soda for sparkling water'? That's not a strategy-that's a Band-Aid. If you're serious about reversing diabetes, you need to go full keto, fast, and do intermittent fasting with 18:6 ratios. And you need to test your ketones daily. Anything less is just self-sabotage. 🙄
Terry Bell
I used to think I had to be perfect. Then I got sick of being tired. So I started walking after dinner. Just 10 minutes. Then I added one veggie to dinner. Then I stopped eating cereal. No apps. No fancy plans. Just small things. Now I sleep better, my knees don't hurt, and I don't feel like I'm fighting my body every day. It's not about losing weight. It's about living better. 🌿
katia dagenais
Why is everyone so obsessed with weight? Why can't we just accept our bodies? I have diabetes and I'm fat. So what? I'm still a person. I'm still worthy. This whole post feels like body-shaming disguised as medicine. I'm tired of being told I'm not trying hard enough. My worth isn't measured in pounds. 💔
Manish Pandya
From India: We’ve been doing this for centuries. Dal, roti, curd, greens, and walking after meals. No counting calories. No fancy apps. Just tradition. My uncle reversed his diabetes at 68 by eating like his grandfather did. Simple. Real. No gimmicks. Maybe we don’t need new science-we need to remember old wisdom. 🙏
Josh Gonzales
Hey, I’m on insulin and lost 22 lbs using the strategies here. My doc lowered my dose by 40%. But I had to check my sugar 5x a day at first-because lows hit hard. If you’re on meds, don’t skip the doctor. Talk to them. Don’t just go off half-cocked. This stuff works, but safety first. 💉