When you pick up your prescription, the pharmacist might say, "We flagged this because of your allergy record." But what does that actually mean? You’re not alone if you’ve been confused by these alerts. They’re everywhere in modern pharmacies and hospitals, popping up on screens during every prescription fill. Most of them are wrong. And that’s the problem.
What Are Pharmacy Allergy Alerts?
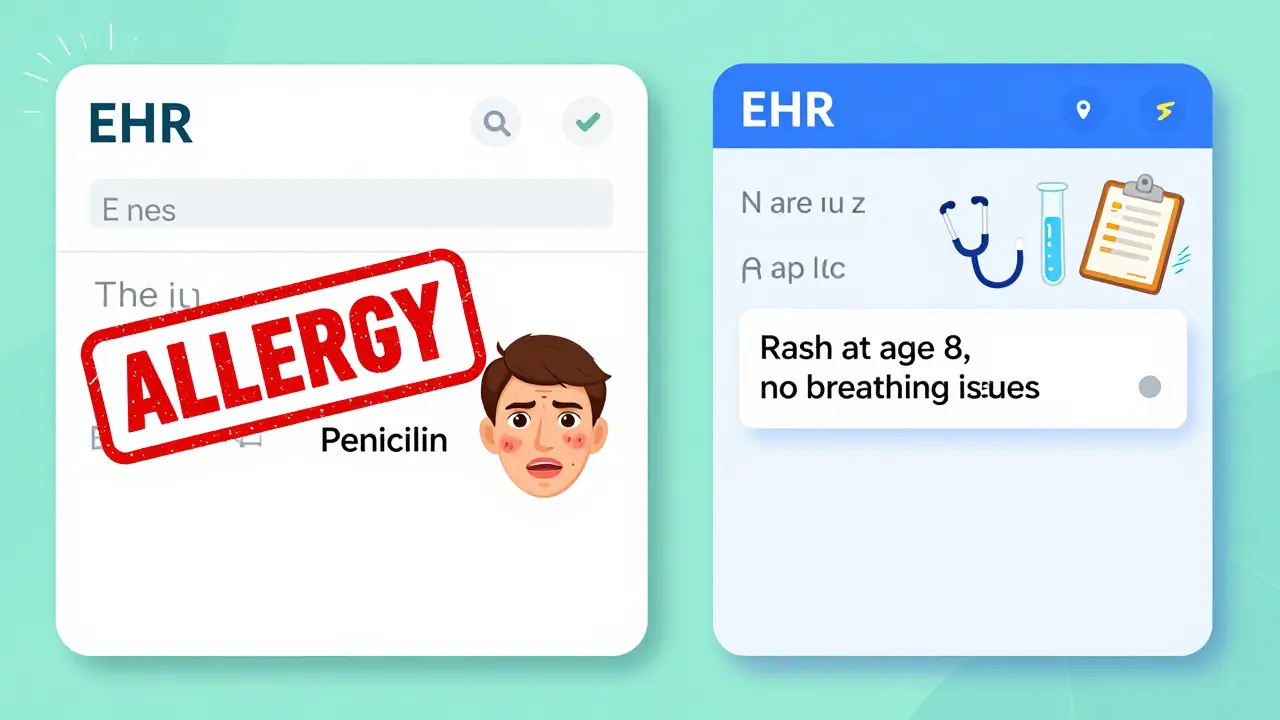
Pharmacy allergy alerts are automated warnings generated by electronic health record (EHR) systems. They pop up when a medication being prescribed or dispensed matches something on your allergy list. These systems were rolled out in the early 2000s to stop dangerous drug reactions. But today, they’re more of a nuisance than a safety net.Here’s how it works: when a doctor orders amoxicillin, the system checks your profile. If it sees "penicillin allergy," it flags it-even if your reaction was a rash at age 8, or you’ve taken penicillin five times since without issue. The system doesn’t know the difference between a real allergy and a side effect like nausea or headache. It just sees a keyword.
According to a 2022 study, 96% of U.S. hospitals use these systems. But here’s the catch: more than 95% of alerts are ignored by clinicians. Why? Because most of them are false alarms.
The Two Types of Alerts You’ll See
Not all alerts are created equal. There are two main types:- Definite allergy alerts: These trigger when the medication is an exact match or part of the same drug class as your documented allergy. For example, if you’re listed as allergic to penicillin and someone orders amoxicillin, this alert fires.
- Possible allergy alerts: These are based on cross-reactivity. For example, if you have a "penicillin allergy," you might get an alert for ceftriaxone-even though the actual risk of reacting to modern cephalosporins is less than 2%.
Here’s the kicker: 90% of all alerts are the second type-possible allergies. And the vast majority of them are unnecessary. A 2019 study in the Annals of Allergy, Asthma & Immunology found that only 12% of NSAID allergy alerts represented real risks. Yet, every single one of them stops the prescription until someone clicks "override."
What the Alert Actually Tells You (and What It Doesn’t)
When an alert pops up, it usually shows three things:- The drug being flagged
- Your documented reaction (e.g., "rash," "anaphylaxis," "stomachache")
- A severity level-often color-coded (yellow, orange, red)
But here’s what’s missing: context. The system doesn’t know if your "penicillin allergy" was a mild rash that went away in two days, or if it was a life-threatening reaction that required an EpiPen. It doesn’t know if you’ve taken the drug safely since 2015. It just sees "allergy" and sounds the alarm.
Real allergic reactions involve your immune system. That’s IgE-mediated-anaphylaxis, hives, swelling, trouble breathing. These are rare. Only 5-10% of reported drug reactions are true allergies. The rest are side effects: nausea from metformin, dizziness from blood pressure meds, stomach upset from antibiotics. But in most EHRs, they’re all lumped together as "allergy."
That’s why a patient with a documented "metformin allergy" (which was actually just diarrhea) gets flagged every time they refill their diabetes script. It’s not just annoying-it’s dangerous. When alerts are ignored too often, real emergencies get missed.
Why Alerts Are So Wrong (And Why You Can’t Trust Them)
The biggest flaw in these systems? They rely on outdated, vague documentation. Most patients don’t know the difference between an allergy and a side effect. They say, "I’m allergic to penicillin," because they got sick after taking it as a kid. But that sickness might’ve been a virus, not an immune response.Studies show that up to 90% of people who think they’re allergic to penicillin aren’t. Yet, their records still say "allergic," and every system in the country treats them like they’re at risk of dying.
Even worse, many EHRs use blanket rules. If you’re allergic to penicillin, you’re automatically flagged for every beta-lactam antibiotic-even ones with almost zero cross-reactivity. Third- and fourth-generation cephalosporins? The real risk is under 2%. But systems still treat them like they’re the same as penicillin.
A 2020 study found that 75-82% of anaphylaxis alerts are overridden-even when the patient truly had a severe reaction. Why? Because clinicians are tired of being interrupted by false alarms. They’ve learned to click through. And that’s a huge safety risk.
How to Actually Read and Use These Alerts
If you’re a patient, here’s what you should do next time you see an alert:- Ask what the alert is for. "Is this because I had a rash, or did I have trouble breathing?"
- Check the reaction description. If it says "nausea," "headache," or "stomach upset," it’s likely not a true allergy.
- Ask if it’s been confirmed. "Has anyone ever tested me for this?" Many people are mislabeled as allergic without ever being properly evaluated.
- Bring your own list. Don’t rely on the pharmacy’s record. Write down what happened, when, and how severe it was. Use simple terms: "Rash after penicillin, age 7. No breathing problems. Took it again in 2020 with no issue."
If you’re a clinician or pharmacist, don’t just override. Ask:
- Is this reaction documented clearly?
- Was it immune-mediated? (Hives, swelling, anaphylaxis)
- When did it happen? True allergies usually occur within minutes to hours-not days later.
- Has the patient taken this drug since?
At Mayo Clinic, they started requiring detailed reaction notes. Within six months, accurate allergy documentation jumped from 39% to 76%. Fewer false alerts. Fewer overrides. Safer care.

What’s Changing-and What You Should Expect
The industry knows these systems are broken. New updates are rolling out:- Risk-stratified alerts: Epic’s 2023 update now scores alerts by likelihood of being real, using machine learning. Low-risk alerts are quieter. High-risk ones demand attention.
- Reaction-specific documentation: More systems now require you to pick from a menu: "hives," "anaphylaxis," "nausea," "rash," etc.-not just "allergy."
- Integration with allergy testing: If you’ve had a drug challenge test or skin test, some systems now auto-update your record and remove false alerts.
By 2026, most major EHRs will use smarter alerting. That means fewer interruptions. Fewer false alarms. And more real protection when you need it.
What You Can Do Today
You don’t have to wait for the system to fix itself. Here’s your action plan:- Review your allergy list at every visit. Ask your doctor: "Is this still accurate?"
- Be specific. Don’t say "I’m allergic to penicillin." Say: "I had a rash after penicillin when I was 8. I’ve taken amoxicillin twice since without issue."
- Request testing if unsure. If you think you’re allergic but aren’t sure, ask for a referral to an allergist. Penicillin allergy testing is safe, quick, and 95% accurate.
- Keep your own record. Use your phone’s notes or a small card. Write down: drug name, reaction, date, severity. Bring it to every appointment.
Medications save lives. But bad alerts can stop them from getting to you. Understanding these warnings isn’t just about reading a screen-it’s about protecting yourself. Don’t assume the system knows better than you. Ask questions. Clarify your history. And don’t let a glitch in a computer program keep you from the medicine you need.
What’s the difference between a drug allergy and a side effect?
A drug allergy is an immune system reaction-like hives, swelling, trouble breathing, or anaphylaxis. Side effects are non-allergic reactions, like nausea, dizziness, or headaches. Most people who think they have a drug allergy actually experienced a side effect. Only 5-10% of reported drug reactions are true allergies.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as a child lose it within 10 years-even if they never got tested. Many people are labeled allergic based on a childhood rash or stomach upset, but later tolerate the drug safely. Testing can confirm if you’re still allergic.
Why do I keep getting alerts for drugs I’ve taken before?
Because your allergy record hasn’t been updated. Most EHR systems don’t auto-correct based on real-world use. If you took amoxicillin twice last year with no reaction, the system still sees "penicillin allergy" and flags it. You need to tell your provider and ask them to update your record.
Are cephalosporins safe if I’m allergic to penicillin?
For most people, yes. The risk of cross-reactivity between penicillin and modern cephalosporins (like ceftriaxone or cefdinir) is less than 2%. Older systems treated all cephalosporins as high-risk, but newer guidelines and software updates now reflect this low risk. If you’ve tolerated a cephalosporin before, it’s very likely safe.
Should I avoid all NSAIDs if I’m allergic to one?
No. Only about 1 in 10 people who react to one NSAID (like ibuprofen) will react to another. Most reactions are side effects, not allergies. If you had stomach upset from Advil, you can likely take naproxen or aspirin safely. But if you had hives or swelling, consult an allergist before trying others.
How can I get my allergy record corrected?
Bring your own written history to your doctor or pharmacist. Say: "I was labeled allergic to penicillin as a child, but I’ve taken it multiple times since with no issue." Ask them to change the record from "allergy" to "intolerance" or "no known allergy." If needed, request a referral to an allergist for testing. Most insurance covers it.
Next Steps for Patients
Don’t wait for your next appointment. Take five minutes now:- Open your pharmacy app or portal and check your allergy list.
- Look at each entry. Is it a true allergy (hives, swelling, breathing trouble)? Or just nausea, dizziness, or a rash that went away?
- If it’s unclear, call your doctor. Ask: "Can we review my allergy list? I think some entries might be wrong."
- Write down your real history. Keep it on your phone. Show it at every visit.
Pharmacy alerts are meant to protect you. But they only work if your record is accurate. You’re the expert on your body. Don’t let a computer make decisions for you-ask questions, clarify your history, and take control.







Philip Leth
Man, I used to get flagged for amoxicillin all the time because my grandma said I was 'allergic' after a rash at five. Turned out I’ve taken it five times since with zero issues. Pharmacies still scream like I’m gonna drop dead. It’s wild how tech outlives common sense.
Just asked my pharmacist last week to update my record - she laughed and said, 'We’ve all seen this a hundred times.' We need better systems, not louder alarms.
Angela Goree
THIS IS WHY AMERICA’S HEALTHCARE IS BROKEN!!
YOU’RE TELLING ME A COMPUTER-A STUPID, DUMB, OVERPRICED SOFTWARE-CAN’T TELL THE DIFFERENCE BETWEEN A RASH AND ANAPHYLAXIS?!
WE’RE PAYING BILLIONS FOR EHRs THAT MAKE US MORE DANGEROUS?!
IF YOU’RE NOT ALLERGIC, STOP SAYING YOU ARE-AND IF YOU ARE, DOCUMENT IT LIKE A HUMAN, NOT A ROBOT!!
Shanahan Crowell
Love this breakdown. Seriously. I work in a clinic and we’ve been pushing for better allergy documentation since 2021. The shift from just typing 'allergy' to selecting 'hives,' 'anaphylaxis,' 'nausea'-it’s a game changer.
One nurse started using a checklist with patients during intake. Within three months, our override rate dropped 40%. People aren’t lazy-they’re just tired of being yelled at by machines that don’t know them.
Kerry Howarth
Simple rule: If it’s not hives, swelling, or breathing trouble, it’s not an allergy. Update your record. Bring your list. Ask for testing. Done.
Stop letting software dictate your care.
Tiffany Channell
Of course the system is broken. It’s designed by bureaucrats who’ve never met a patient. The real problem isn’t the algorithm-it’s the cultural ignorance. People don’t know the difference between side effects and immune responses because medicine stopped teaching basic immunology decades ago.
And now we’re stuck with a generation of patients who think 'allergy' means 'I felt weird once.'
It’s not a glitch. It’s a symptom of systemic decay.
Joy F
Think about it: we’ve outsourced our bodily intuition to machines that don’t understand context, nuance, or the sacred chaos of human biology.
That alert? It’s not a warning-it’s a capitalist echo chamber. A corporate checkbox dressed up as safety. We’ve turned healing into a compliance ritual.
And the worst part? We’ve normalized it. We click 'override' like it’s a TikTok like. We’ve surrendered our agency to a UI that doesn’t care if we live or die.
It’s not about penicillin. It’s about control. Who gets to decide what your body can tolerate?
Not the algorithm. Not the pharmacist. Not even the doctor.
You.
And you’ve forgotten that.
Haley Parizo
My mom’s allergy list says 'penicillin' because she got a rash at 12. She’s 72 now. She’s taken it 17 times since. No issues. But every time she fills a script, the pharmacy stops everything. I’ve had to call them five times just to get them to update a damn record.
This isn’t healthcare. It’s bureaucratic theater. And we’re all actors in a play written by people who’ve never held a stethoscope.
Ian Detrick
Just got my penicillin skin test done last month. Turned out I’m not allergic. Took amoxicillin last week. Felt great.
Wish I’d done this 15 years ago. So many antibiotics I avoided, so many worse drugs I was forced into.
Test if you’re unsure. It’s quick, safe, and free with most insurance.
Don’t let a childhood mistake haunt your adult prescriptions.
Lori Jackson
It’s fascinating how people romanticize their own ignorance as 'personal knowledge.'
You didn't 'have a rash'-you had an immune response. Or you didn't. There’s no in-between. But you’d rather cling to the comforting lie that 'I know my body' than admit you’ve never been properly evaluated.
And now you expect a pharmacist-who’s been trained to trust the system-to gamble your life on your anecdote?
Stop being emotionally manipulative. Get tested. Or shut up.
Wren Hamley
Biggest myth: 'I’m allergic to NSAIDs.'
Turns out, if you got stomach cramps from ibuprofen, you’re probably not allergic-you’re just sensitive. But the system sees 'NSAID allergy' and blocks naproxen, celecoxib, even aspirin.
It’s like banning all fruits because one gave you a tummy ache.
Fun fact: 90% of people who think they’re allergic to NSAIDs can take another one safely. But no one ever asks. We just accept the warning like it’s gospel.
Question everything. Especially the machine.
Sarah Little
Can I ask-what’s the process to get your allergy record updated? I’ve called my doctor three times. They say, 'Just come in.' But I’m working two jobs. I don’t have time to sit in a waiting room for an hour to fix a typo in a computer.
And if I call the pharmacy, they say, 'We can’t change that.'
So who’s supposed to fix this? The system is broken, but no one’s accountable.
I’m not lazy. I’m just stuck.
innocent massawe
Same here in Nigeria. We don’t even have proper EHRs-but when we do, I hope they learn from U.S. mistakes.
My cousin was labeled penicillin allergic because he got diarrhea after taking it as a kid. Now he’s on expensive, weaker antibiotics because no one checks.
Maybe the real problem isn’t the tech-it’s that we don’t teach people how to talk about their bodies.
Simple words. Clear history. That’s all it takes.