Formulary Tiers Explained: How Your Insurance Decides What Medications Cost
When you pick up a prescription, the price you pay isn’t just set by the drug company—it’s decided by your formulary tiers, a system used by insurance plans to group medications by cost and coverage. Also known as a drug formulary, this list tells your pharmacy benefit manager (PBM) which drugs to cover, and how much you’ll pay for each one. It’s not about which drug works best—it’s about which one your plan says is worth covering at each price level.
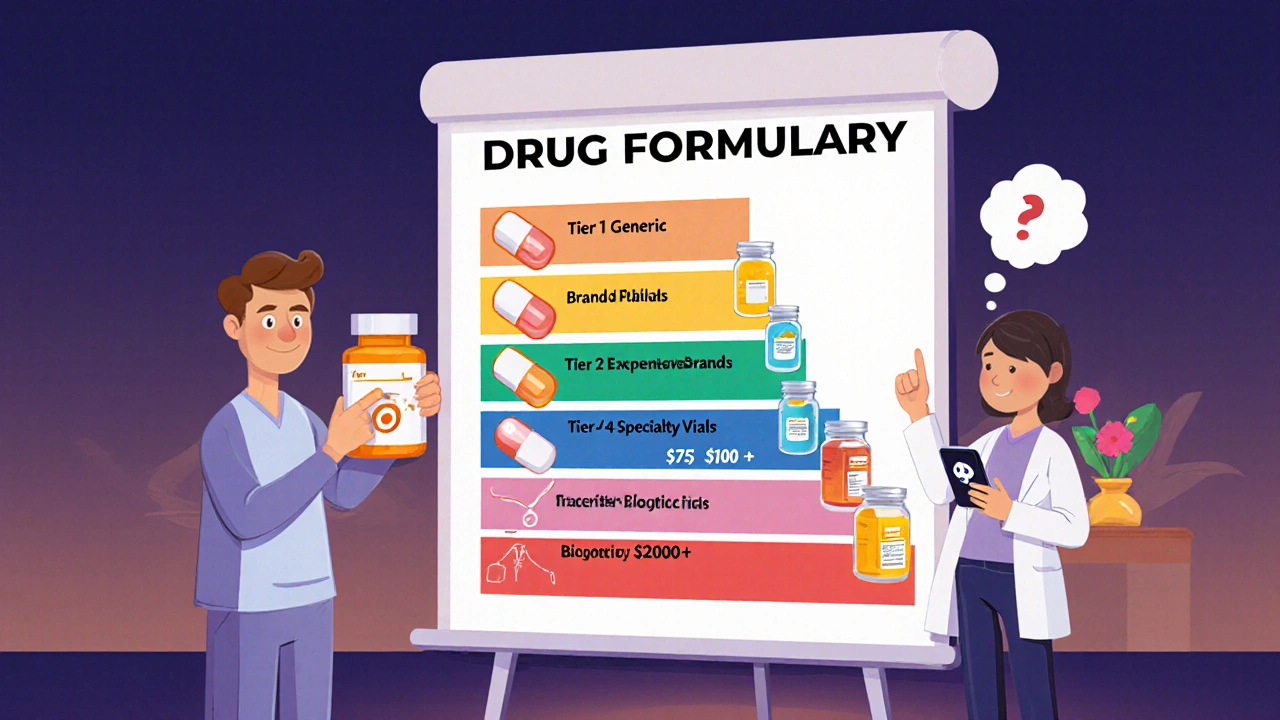
Formulary tiers exist because insurers need to control costs. They put cheaper, generic drugs on the lowest tier—Tier 1—so you pay just $5 or $10. Then come brand-name drugs that don’t have generics yet, usually Tier 2. Higher tiers like Tier 3 and Tier 4 include expensive specialty drugs, sometimes costing hundreds. And then there’s Tier 5, where drugs like those for hepatitis C or rare cancers can run over $1,000 a month. Your plan might require you to try cheaper options first before approving the pricier ones—that’s called step therapy, and it’s built right into how formulary tiers work.
Not all drugs are treated the same, even if they do the same job. Take ibuprofen and diclofenac—both are anti-inflammatories. But if your plan lists ibuprofen on Tier 1 and diclofenac on Tier 3, you’ll pay way more for the latter, even if your doctor says it works better for you. Same goes for levothyroxine versus a brand-name thyroid med. One’s a generic, the other’s not—and your wallet feels the difference. Even antihistamines like loratadine and diphenhydramine can be split across tiers, depending on whether your plan considers them "preferred." And when you’re managing something like diabetes, the difference between Tier 2 and Tier 4 can mean hundreds of dollars a month on meds like metformin or SGLT-2 inhibitors.
It’s not just about price. Formulary tiers also affect what your doctor can prescribe. If your plan won’t cover a drug unless you fail two others first, you’re stuck jumping through hoops. That’s why knowing your formulary tiers helps you ask better questions. Can we switch to a Tier 1 alternative? Is there a patient assistance program? Should I check with my pharmacy if they have a cheaper cash price? These aren’t just money questions—they’re safety questions too. A 2021 study found that patients who couldn’t afford their meds were 2.5 times more likely to skip doses. That’s not just inconvenient—it’s dangerous.
Behind every tier is a decision made by your insurer’s pharmacy benefit manager, not your doctor. And while these lists change often, they rarely come with an explanation. That’s why we’ve gathered real stories and facts from people who’ve been there—like those who had to switch from Foracort Inhaler to a cheaper alternative because their plan moved it to a higher tier, or those who nearly missed their levothyroxine dose because they didn’t know calcium supplements could block absorption. You’ll find guides on how to appeal a denial, how to spot when a drug moves tiers, and how to use tools like visual dosing aids to avoid mistakes when switching meds. Whether you’re juggling medication safety, dealing with a drug shortage, or just trying to make sense of your co-pay, understanding formulary tiers gives you real power. Below, you’ll find practical advice from people who’ve navigated these systems—and learned how to get the care they need without going broke.
A drug formulary is your insurance plan's list of covered medications. Learn how tiers, exceptions, and new 2025 rules affect your out-of-pocket costs and how to find the best coverage for your prescriptions.