Why Antipsychotics Can Change Your Metabolism
Antipsychotic medications help manage serious mental health conditions like schizophrenia and bipolar disorder. But for many people, the benefits come with a hidden cost: serious metabolic changes. These drugs don’t just affect thoughts and moods-they can trigger weight gain, high blood sugar, and unhealthy cholesterol levels. In fact, up to 68% of people taking second-generation antipsychotics develop metabolic syndrome, compared to just 3.3% in the general population. This isn’t a rare side effect. It’s common, predictable, and often overlooked.
The Real Risk: More Than Just Weight Gain
When doctors talk about metabolic risks from antipsychotics, they’re not just warning about the scale going up. They’re talking about a cluster of dangerous changes: waist size growing, triglycerides climbing, HDL (good cholesterol) dropping, blood pressure rising, and fasting glucose spiking. Together, these make up metabolic syndrome. People with this condition are three times more likely to have a heart attack or stroke. And the risk doesn’t wait years to show up. Blood sugar and fat levels can start shifting within weeks-even before noticeable weight gain.
Not All Antipsychotics Are the Same
Some antipsychotics are much harder on your metabolism than others. Olanzapine and clozapine are the worst offenders. In the CATIE study, people on olanzapine gained an average of 2 pounds per month. Nearly one-third gained a dangerous amount of weight in just 18 months. Clozapine isn’t far behind. Both drugs are powerful for treatment-resistant psychosis, but they come with heavy metabolic baggage.
On the other side, ziprasidone, lurasidone, and aripiprazole show far less impact. People on these medications often see little to no weight gain and stable blood sugar levels. Risperidone and quetiapine fall in the middle-they can cause moderate changes, but not as severe as olanzapine. Choosing the right drug isn’t just about controlling symptoms. It’s about protecting your long-term health.
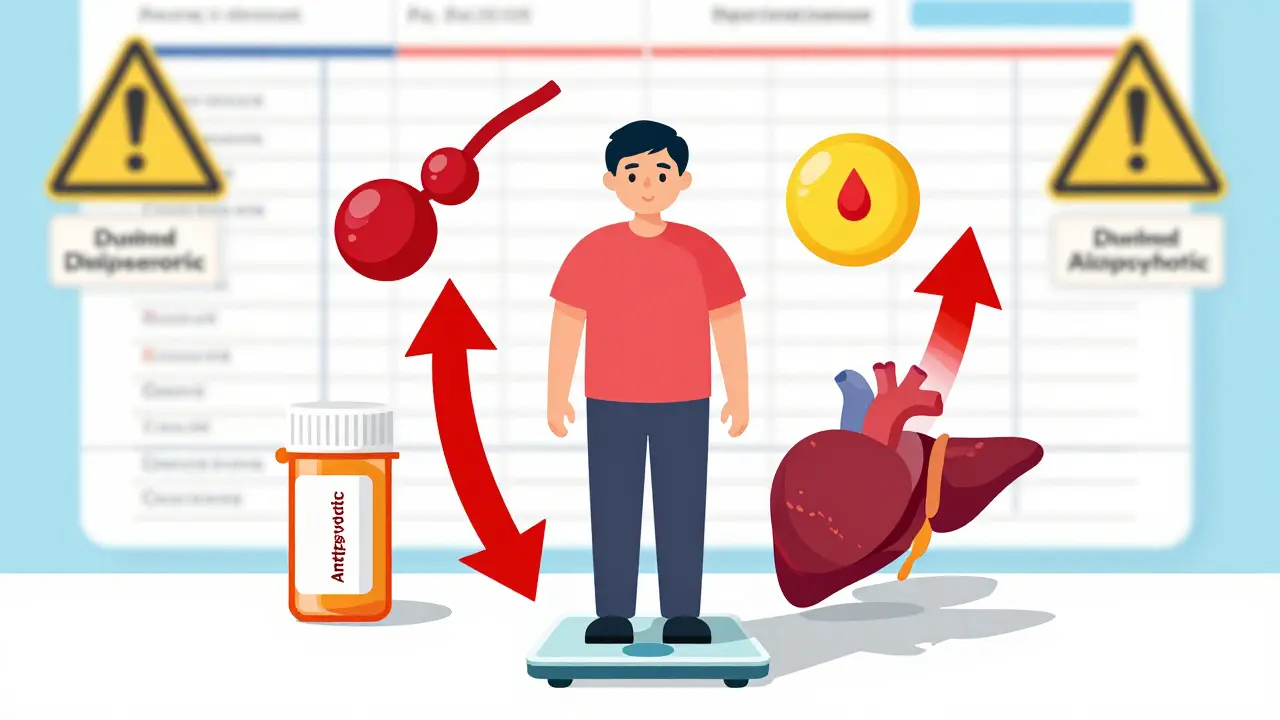
How These Drugs Break Down Your Metabolism
It’s not just about appetite. Antipsychotics interfere with how your body handles energy at a cellular level. They mess with signals in the brain that control hunger and fullness. They also directly affect your liver, pancreas, fat cells, and muscles. This means your body starts storing fat more easily, even if you eat the same amount. Your pancreas may struggle to release insulin properly. Your liver begins producing more triglycerides. And your muscles become less sensitive to insulin, leading to high blood sugar.
Some research suggests these drugs might even damage mitochondria-the energy factories inside your cells. This could explain why weight gain and diabetes happen so fast, even in people who don’t overeat. The damage starts before you notice it.
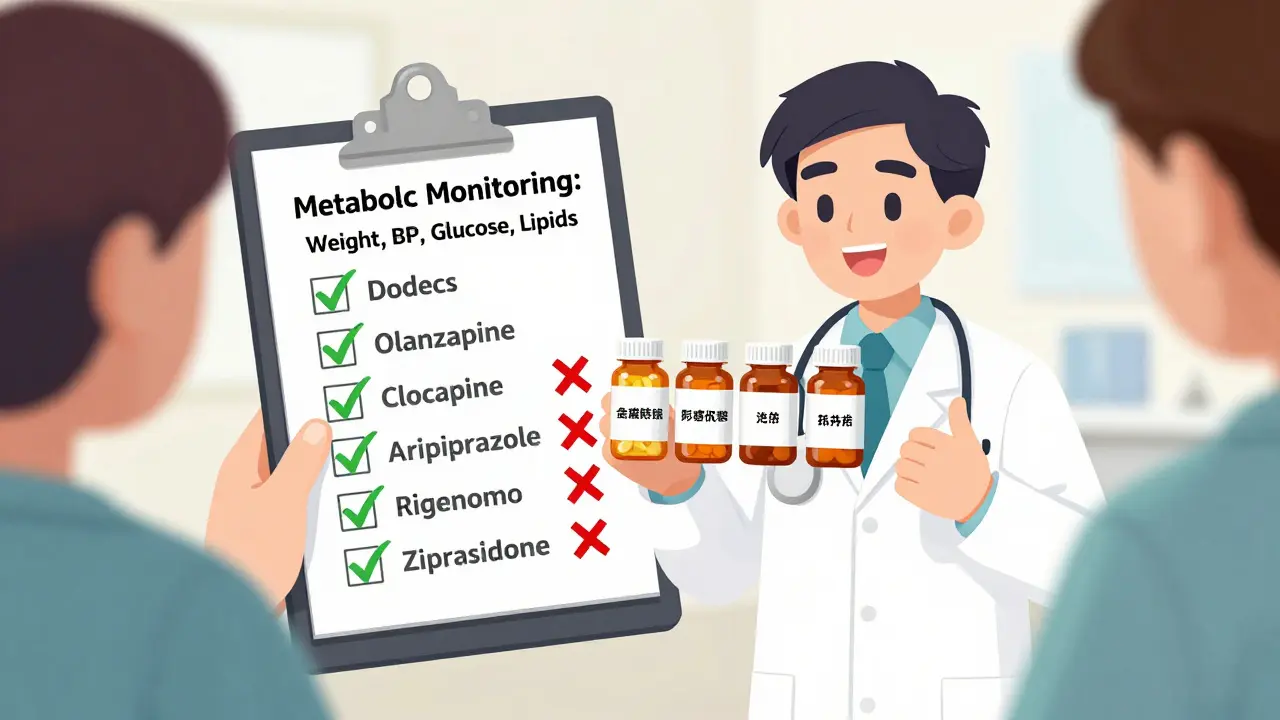
Monitoring Is Not Optional
Guidelines from the American Psychiatric Association and the American Diabetes Association are clear: every person starting an antipsychotic needs baseline metabolic testing. That means checking your weight, waist size, blood pressure, fasting blood sugar, and lipid panel before you even take your first pill.
After that, follow-up tests are critical:
- At 4 weeks: Check weight and blood pressure
- At 12 weeks: Repeat blood sugar and lipids
- At 24 weeks: Full metabolic panel again
- Every 3 to 12 months after that: Ongoing monitoring
Even if you feel fine, these tests catch problems early. Many patients don’t realize their blood sugar is rising until they’re already pre-diabetic. By then, reversing it is much harder.
What Happens When Monitoring Is Ignored
Too often, metabolic checks are skipped. Clinicians focus on psychosis symptoms and assume weight gain is just "a side effect you have to live with." But this mindset costs lives. People on long-term antipsychotics die 15 to 20 years earlier than the general population-mostly from heart disease and diabetes. And in many cases, those deaths were preventable.
One study found that nearly half of patients on antipsychotics had never had their cholesterol checked. A third had no record of blood pressure monitoring. This isn’t negligence-it’s a systemic failure. Patients need advocates. If your doctor doesn’t mention metabolic testing, ask for it.
What You Can Do to Protect Yourself
Medication alone isn’t enough. Lifestyle changes make a real difference. A structured diet and regular exercise can cut weight gain in half for people on antipsychotics. You don’t need a gym membership. Walking 30 minutes a day, five days a week, helps. Cutting sugary drinks and processed carbs matters more than counting calories.
Some patients benefit from medications that target metabolic side effects-like metformin for insulin resistance or statins for high cholesterol. These aren’t alternatives to antipsychotics. They’re supports. Talk to your doctor about whether they’re right for you.
And if you’re struggling with weight gain on a high-risk drug like olanzapine or clozapine, don’t assume you’re stuck. With psychiatric guidance, switching to a lower-risk antipsychotic is often possible. It’s not a failure. It’s smart management.

Long-Acting Injections Don’t Help
Some patients think switching to a long-acting injectable (LAI) form will reduce metabolic risks. It won’t. The drug is still the same. Whether you swallow a pill or get a shot, your body processes it the same way. Monitoring stays just as important.
Why This Matters Beyond the Clinic
Metabolic side effects are the #1 reason people stop taking their antipsychotics. One study found that 20% to 50% of patients quit because of weight gain, fatigue, or feeling unwell. That’s not just a personal problem-it leads to relapse, hospitalization, and loss of independence. When you protect your metabolism, you protect your ability to stay stable, work, and live your life.
This isn’t about being perfect. It’s about awareness. If you’re on an antipsychotic, you’re at higher risk for heart disease and diabetes. That doesn’t mean you can’t take the medication. It means you need to take care of your body just as seriously as you take your pills.
What’s Next?
Research is moving fast. Scientists are testing new drugs that block the metabolic side effects without reducing the antipsychotic benefits. Some are even looking at supplements and timing of meals to reduce insulin spikes. But for now, the best tools we have are simple: know your numbers, move your body, eat real food, and speak up if something feels off.
Antipsychotics save lives. But they can also shorten them-if we don’t pay attention to the whole picture. Your mental health matters. So does your heart, your liver, and your blood sugar. They’re all connected.
Do all antipsychotics cause weight gain?
No. While many antipsychotics-especially olanzapine and clozapine-cause significant weight gain, others like aripiprazole, lurasidone, and ziprasidone have much lower risks. Some patients gain only a pound or two, or none at all. The key is choosing the right medication based on your health history and monitoring changes early.
How soon after starting antipsychotics do metabolic changes begin?
Metabolic changes can start within the first few weeks. Blood sugar and triglyceride levels often rise before noticeable weight gain occurs. That’s why initial testing at 4 and 12 weeks is so important. Waiting until you see weight gain means you’re already behind.
Can I stop my antipsychotic if I gain weight?
Never stop your medication without talking to your psychiatrist. Stopping suddenly can trigger psychosis relapse, which is far more dangerous than weight gain. Instead, work with your doctor to adjust your treatment plan. You might switch to a lower-risk drug, add metformin, or start a structured diet and exercise program.
Is metabolic monitoring covered by insurance?
Yes. Basic metabolic tests-like fasting glucose, lipid panels, and blood pressure checks-are routinely covered under most insurance plans as preventive care. If your provider says no, ask for a written explanation. These tests are not optional; they’re standard of care according to major medical associations.
Can exercise and diet reverse antipsychotic-induced metabolic damage?
Yes, in many cases. Studies show that even modest lifestyle changes-like losing 5% of body weight, walking 150 minutes a week, and cutting sugary foods-can improve insulin sensitivity, lower triglycerides, and reduce blood pressure. The earlier you start, the better the results. It’s not a cure, but it’s a powerful tool to reduce long-term risk.
Why don’t more doctors monitor metabolic health?
Many clinicians are focused on managing psychiatric symptoms and may not have time, training, or systems in place for routine metabolic checks. Some still believe weight gain is an unavoidable side effect. But guidelines have been clear for over a decade. Patients should advocate for themselves-if your doctor hasn’t ordered a lipid panel or checked your waist circumference in the past year, it’s time to ask why.








Colin Pierce
Just wanted to say this is one of the clearest breakdowns I’ve seen on this topic. I’ve been on risperidone for 5 years and only found out last year my triglycerides were through the roof because no one ever checked. Starting metformin and walking daily cut my numbers in half. You’re not alone, and it’s never too late to turn things around.
fiona vaz
My sister was on olanzapine for 18 months and gained 60 pounds. They never monitored her glucose or lipids. She had a stroke at 34. This isn’t just about weight-it’s survival. Please, if you’re on these meds, demand the tests. No excuses.
John Rose
It’s wild how much we’re expected to just accept this as ‘part of the deal.’ I’m on aripiprazole now-zero weight gain, stable sugars. The difference is night and day. If your doctor doesn’t bring up metabolic health, it’s not because it’s unimportant-it’s because they’re overwhelmed. Be your own advocate.
Lance Long
THIS. THIS RIGHT HERE. I spent years thinking I was lazy, weak, broken-because I gained weight on clozapine. Turns out my mitochondria were being sabotaged by the very thing keeping me alive. I started walking after dinner, swapped soda for sparkling water, and now my A1C is normal. It’s not magic. It’s science. And you deserve to live long enough to see the sun rise without fear.
Sue Latham
Ugh. I can’t believe people still think ‘just eat less’ fixes this. Like, wow. You clearly don’t understand how these drugs rewire your biology. It’s not willpower. It’s pharmacology. Stop blaming patients. Fix the system.
Bryan Fracchia
There’s a quiet tragedy here: we treat the mind, but forget the body is still a temple. These drugs don’t just alter thoughts-they alter the very rhythm of life inside us. The fact that we don’t treat metabolic health as part of psychiatric care says more about our priorities than about the illness. Maybe healing isn’t just about silence-it’s about balance. And balance requires seeing the whole person.
Amber Daugs
Wow, I’m shocked anyone would even consider skipping metabolic testing. Are we really still in the 1990s? This isn’t rocket science. Check weight, check glucose, check lipids. If your doctor isn’t doing this, find a new one. You’re not being ‘difficult’-you’re being responsible. And if you’re not, you’re risking your life for a symptom.
Mark Alan
WHY ISN’T THIS ON THE NEWS?!?!? 😭💔 I’m so angry right now. My cousin died at 32 from a heart attack because they didn’t check his cholesterol. He was on quetiapine. He was 27. This is a MASSIVE COVER-UP. #MetabolicMurder #AntipsychoticsAreKillingUs
James Dwyer
My doctor didn’t mention any of this until I brought it up. Now I get labs every 3 months. I’m on lurasidone. No weight gain. No drama. Just stability. If you’re on a high-risk med and not being monitored-you’re not being cared for. Ask for your numbers. They’re yours to know.