When you switch health plans, your monthly premium isn’t the only thing that changes. Your generic drug coverage might look the same on paper-but it could cost you hundreds more each year if you don’t check the details. Many people assume all generics are treated equally, but that’s not true. A $3 copay for metformin in one plan could become a $40 coinsurance in another-even if it’s the exact same drug. And if you take multiple prescriptions, those differences add up fast.
Why Generic Drug Coverage Matters More Than You Think
Generic drugs make up 90% of all prescriptions filled in the U.S., but they only account for about 23% of total drug spending. That’s because they’re cheaper to produce and insurers negotiate lower prices. But here’s the catch: not all plans treat them the same. Some charge a flat $5 copay. Others make you pay a percentage of the drug’s price after you hit a deductible. And some don’t cover your specific brand of generic at all.Take levothyroxine, a common thyroid medication. One plan might cover Synthroid’s generic (made by Teva) as a Tier 1 drug with $0 copay. Another plan might only cover the version made by Mylan and classify it as Tier 2-meaning you pay 25% of the cost. Same active ingredient. Same FDA approval. Different price. That’s the reality of formularies.
According to CMS data from 2023, 84% of all prescriptions filled were for generics. But if your plan doesn’t cover the one you need, you’re stuck paying full price-or switching meds. That’s why checking your specific drugs before switching plans isn’t optional. It’s essential.
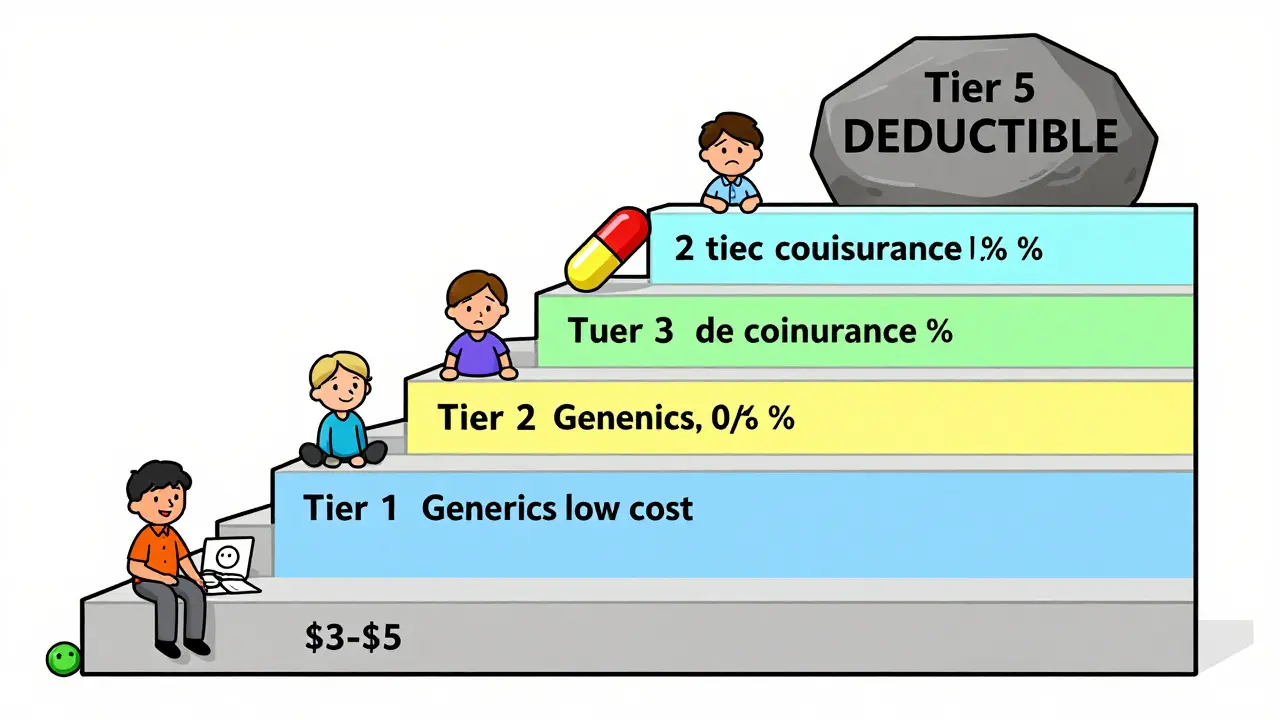
How Formularies Work: The Tier System Explained
Most health plans use a tiered system to organize drugs. The lower the tier, the less you pay. Here’s how it usually breaks down:- Tier 1: Preferred generics. These are the cheapest. Copays range from $3 to $20 for a 30-day supply.
- Tier 2: Non-preferred generics or brand-name drugs with generic alternatives. Copays jump to $20-$50.
- Tier 3: Preferred brand-name drugs. Often no generic available yet. Coinsurance (like 20-30%) kicks in.
- Tier 4: Non-preferred brands or specialty drugs. Could be 40% coinsurance or more.
- Tier 5 (in some plans): High-cost specialty generics or biologics. May require prior authorization.
Medicare Part D and employer plans often have 4 or 5 tiers. Marketplace plans (like those on Healthcare.gov) are required to use a 4-tier structure under federal rules. But here’s where it gets tricky: some plans combine your medical deductible with your drug deductible. That means you might have to pay $2,000 out of pocket for doctor visits before your $5 generic copay even starts.
That’s why Silver Standardized Plan Design (SPD) plans are a game-changer. In 2023, these plans waived the deductible for Tier 1 generics and kept copays at $20 or less. If you take daily meds like blood pressure or diabetes drugs, this could save you over $1,500 a year compared to a non-SPD plan.
What to Check Before Switching Plans
Don’t just glance at the plan summary. Dig into the details. Here’s your checklist:- Get the full formulary. Don’t rely on a “preferred drugs” list. Download the complete drug list from the insurer’s website. Look for your exact medication name and manufacturer.
- Match the formulation. Is your prescription metformin ER (extended release)? Some plans only cover immediate-release versions. Even if the active ingredient is the same, the formulation matters.
- Check the tier. Is your drug in Tier 1? If not, how much will you pay? Is it a copay or coinsurance? Coinsurance means you pay a percentage of the drug’s cost-which can spike if the price goes up.
- Verify your pharmacy. Your local CVS might be in-network. But what about the pharmacy you use for mail-order? Some plans charge 300-400% more if you use a non-preferred pharmacy.
- Calculate your annual cost. Multiply your monthly copay by 12. Add any deductible you must meet first. Then compare that to your current plan. Don’t forget: if you take 3 or more meds, those costs stack up.
For example, if you take metformin 500mg (Tier 1, $5 copay), lisinopril (Tier 1, $10 copay), and atorvastatin (Tier 1, $3 copay), your annual cost under a good plan would be $216. Under a bad one-with $20 copays and a $1,000 deductible-you could pay $1,800 before coverage kicks in. That’s an extra $1,584.
State Rules Can Change Everything
Your state isn’t just a location-it’s a policy engine. California requires a $85 outpatient drug deductible before coverage starts, then charges 20% coinsurance up to a $250 cap. New York waives the deductible entirely for generics and caps copays at $75 for specialty drugs. DC has a separate $350 drug deductible. These differences aren’t minor. They can make one plan 50% cheaper than another-even if they’re from the same insurer.And don’t forget insulin. Thanks to the Inflation Reduction Act, Medicare beneficiaries now pay no more than $35 per month for insulin. But this only applies to Part D plans. If you’re on a private plan, check if your state has similar caps. California, New Jersey, and Illinois now require $0 insulin copays for all plans.
Tools That Actually Work
There are free tools built to help you compare. Use them.- Medicare Plan Finder (medicare.gov): Enter your drugs, zip code, and pharmacy. It shows you the total annual cost for every Part D plan in your area. Used by over 4 million people in 2022.
- Healthcare.gov Plan Selector: Filters plans by formulary and shows estimated drug costs. Look for the “Drug Coverage” tab.
- Insurer-specific tools: Blue Cross, UnitedHealthcare, and others have online formulary checkers. Accuracy varies, but insurer sites are usually 96% accurate compared to 78% on third-party tools.
- Medicare Plan Scout (beta): A new CMS-endorsed AI tool launched in 2023. It cut enrollment errors by 44% in testing. Try it if you’re on Medicare.
One user in Ohio switched from a $15 generic copay plan to one with $3 copays after using the Medicare Plan Finder. She saved $780 a year on her three maintenance drugs. That’s not luck-that’s due diligence.

Common Mistakes People Make
Most people who end up paying more after switching make the same three errors:- Assuming all generics are equal. A generic isn’t just a generic. The manufacturer matters. If your plan drops your current maker, you could be forced into a higher tier.
- Ignoring mail-order rules. Some plans charge double at retail pharmacies but offer $0 copays for 90-day mail-order fills. If you’re on a fixed income, that’s a big deal.
- Not checking for formulary changes. Insurers update formularies every year. A drug that was Tier 1 in December could be Tier 3 in January. Always verify during open enrollment.
Reddit’s r/healthinsurance had 147 documented cases in 2023 where people paid hundreds extra because their generic switched manufacturers. One person’s levothyroxine went from $0 to $45 a month because the new plan only covered a different brand. They didn’t know until they filled the prescription.
What to Do If Your Drug Isn’t Covered
If your medication isn’t on the formulary, you have options:- Ask for a formulary exception. Submit a request to your insurer. Include a letter from your doctor explaining why you need this specific drug. Many requests get approved, especially for chronic conditions.
- Try a therapeutic alternative. Your doctor might be able to switch you to a similar drug that’s covered. For example, if your generic statin isn’t covered, another one might be.
- Use a patient assistance program. Many drugmakers offer free or low-cost generics to people with low income. Check NeedyMeds.org.
Don’t assume you’re stuck. In 2022, CMS reported that 68% of formulary exception requests for generic drugs were approved when supported by medical documentation.
Final Tip: Do This Every Year
Your health plan changes every year. So should your evaluation. Even if you’re happy with your current plan, review your formulary during open enrollment. A small change-like a new manufacturer or a new deductible rule-can cost you money. Set a reminder for October. Take 20 minutes. Run your drugs through the plan finder. Compare. Switch if needed.People who do this save an average of 25-40% on their prescription costs. That’s not just smart. It’s necessary.
How do I find out if my generic drug is covered by a new health plan?
Download the full formulary from the insurer’s website-not just a summary. Search for your exact drug name, including the manufacturer (e.g., metformin by Teva). Then check the tier. Tier 1 means lowest cost. If it’s not listed, call customer service and ask if it’s covered under an exception.
Are all generic drugs the same, or does the manufacturer matter?
The active ingredient is the same, but manufacturers can differ in fillers, coatings, or release timing. Some plans only cover specific brands. For example, one plan might cover metformin from Mylan but not Teva-even though both are FDA-approved. Always verify the manufacturer on the formulary.
What’s the difference between a copay and coinsurance for generics?
A copay is a fixed amount you pay-like $5 per prescription. Coinsurance is a percentage of the drug’s cost-like 20%. Coinsurance can be unpredictable because drug prices change. A $5 copay is always $5. A 20% coinsurance on a $100 drug is $20. Always prefer copays over coinsurance when possible.
Do I have to meet a deductible before my generic drug copay kicks in?
It depends. In Silver Standardized Plan Design (SPD) plans, you don’t-Tier 1 generics have fixed copays even before you meet your deductible. In other plans, especially high-deductible ones, you must pay the full deductible for medical and drug costs before any coverage applies. Always check the plan’s summary of benefits.
Can I switch plans mid-year if my generic drug gets dropped?
Generally, no-unless you qualify for a Special Enrollment Period. If your plan drops your drug mid-year, you can request a formulary exception. If denied, you may qualify for a Special Enrollment Period based on loss of coverage. Contact your state’s insurance department or Medicare for guidance.
Are there any free tools to compare generic drug costs between plans?
Yes. Medicare.gov’s Plan Finder is free and accurate for Medicare Part D. Healthcare.gov’s plan selector works for marketplace plans. Insurer websites like Blue Cross or UnitedHealthcare also have their own formulary checkers-these are often the most accurate. Avoid third-party tools that aren’t tied to official databases.











swati Thounaojam
just checked my plan and my metformin went from $3 to $25 😭 why is this even a thing?
Ken Porter
Stop acting like this is new. Insurance companies have been screwing people over with generics since the 90s. If you can't read a formulary, you deserve to pay more.
Donny Airlangga
I used to think all generics were the same until my thyroid med switched manufacturers and I started having panic attacks. Turns out the fillers matter more than we're told. Never skip checking the brand.
Molly Silvernale
It's not just about dollars-it's about dignity. You're not a statistic, you're a person who needs to breathe, think, and live without choosing between insulin and groceries. And yet, the system treats your survival like a spreadsheet equation.
Kristina Felixita
OMG YES I just did this last week!! I was on a plan that covered my levothyroxine from Teva, switched to a 'cheaper' one, and then got billed $47 for my monthly script 😭 turned out they only covered Mylan, which my body hates. Called my doc, got a prior auth, saved my sanity. You guys, check the manufacturer!!!
Joanna Brancewicz
Coinsurance vs. copay is a critical distinction in formulary architecture. The variability in cost-sharing mechanisms introduces significant financial toxicity for polypharmacy patients, especially under high-deductible health plans with non-tiered drug structures.
Evan Smith
So let me get this straight… I have to Google my drug’s manufacturer and then call my insurer to find out if they hate my pills? And this is normal? 😅
Lois Li
People don't realize how much this affects mental health too. I had to stop my antidepressant because my new plan didn't cover the generic I'd been on for 5 years. Took me 3 months to get it back. Don't underestimate how much stability these meds give you.
christy lianto
THIS. This is why I spend 3 hours every November comparing plans. I have 4 meds. One wrong choice = $1,800 extra. I don't care if it's 'boring'-I'm not risking my health on a gamble. Do the work. Your future self will thank you.
Annette Robinson
If you're on Medicare, use the Plan Finder. It's free, accurate, and it literally saved me $1,200 last year. Just type in your drugs, your pharmacy, and let it do the math. No excuses.
Luke Crump
They say generics save money. But who’s really saving? Not you. Not me. The shareholders. The CEOs. The insurance lobbyists. We’re just the lab rats in their drug pricing experiment.
Manish Kumar
Let me tell you something about the Indian healthcare system-here, generics are not just affordable, they're the *only* option. But even there, the quality varies wildly. Some brands use talc instead of lactose, and patients get rashes. So when you say 'same active ingredient,' you're ignoring the excipients. Those aren't inert-they're the silent killers. In India, we call it 'pharma roulette.' In America, you just call it 'insurance.' Same game, different stakes.
Aubrey Mallory
Anyone who says 'just switch plans' doesn't live with chronic illness. It’s not a switch-it’s a whole new medical bureaucracy. I’ve had to re-file prior authorizations three times just to get back on the same generic. Don’t tell me to ‘do the research.’ I’ve already lost three days of work doing it.