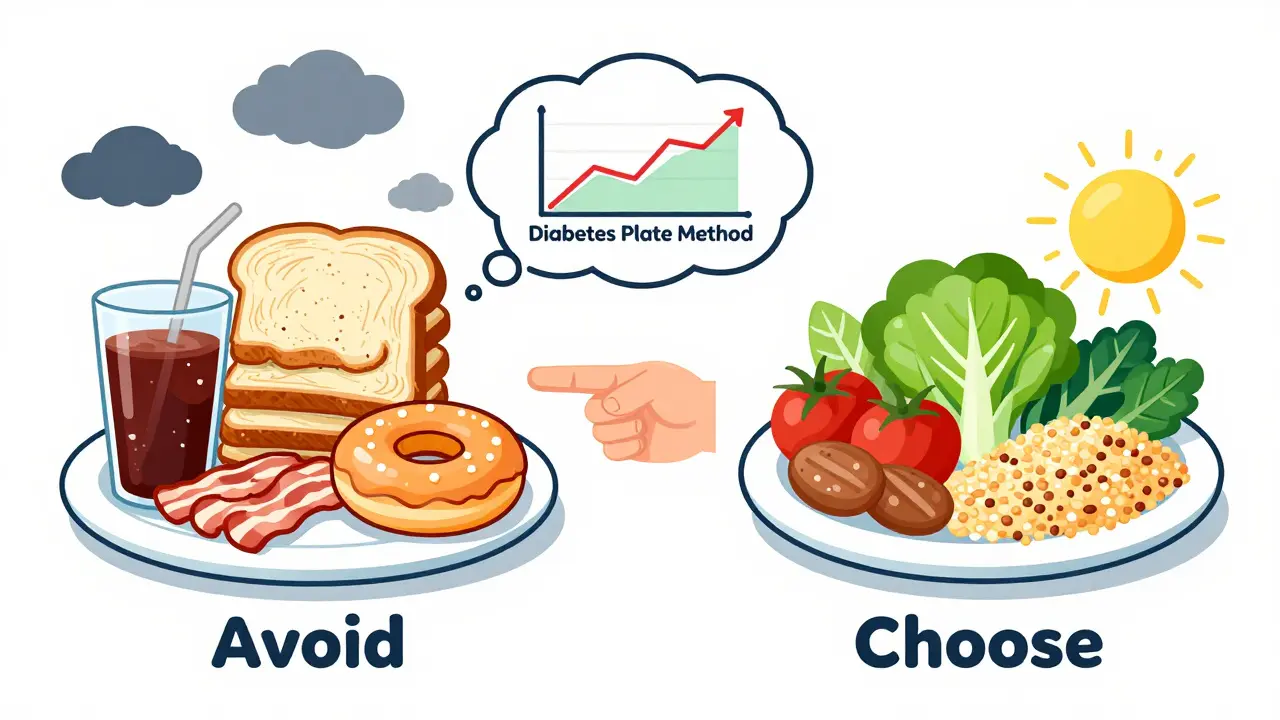
Managing diabetes isn’t about cutting out all your favorite foods-it’s about making smarter choices that keep your blood sugar steady. If you’re trying to figure out what to eat and what to skip, you’re not alone. Millions of people with diabetes are doing the same thing. The good news? You don’t need to count every carb or starve yourself. A simple, science-backed method called the Diabetes Plate Method works better than complicated diets for most people.
How the Plate Method Works
The Diabetes Plate Method is the easiest way to build a meal that helps control blood sugar without counting calories or carbs. All you need is a 9-inch plate-the size of a standard dinner plate or a business envelope. Divide it like this:- Half the plate: Non-starchy vegetables. Think broccoli, spinach, carrots, bell peppers, zucchini, mushrooms, or a big green salad. These are low in carbs and high in fiber, so they fill you up without spiking your blood sugar.
- One-quarter of the plate: Lean protein. Choose skinless chicken, turkey, fish (especially salmon or sardines), tofu, eggs, or beans. Protein helps you stay full and slows down how fast carbs are absorbed.
- The last quarter: Carbohydrates. Pick whole grains like quinoa, barley, or brown rice. Or go for starchy vegetables like sweet potatoes, corn, or peas. You can also include a small piece of fruit or a serving of low-fat dairy like plain yogurt or milk.
This method doesn’t require a scale or app. Just use your hand as a guide: a 3-ounce portion of meat is about the size of your palm, a tablespoon of peanut butter is the tip of your thumb, and a cup of fruit fits in your fist. It’s simple, visual, and works whether you’re eating at home or ordering takeout.
Foods to Eat: The Real Winners for Blood Sugar
Not all carbs are bad. The key is choosing the right kind. Here’s what actually helps:- Non-starchy vegetables: These are your best friends. Broccoli, kale, cucumbers, asparagus, and tomatoes have minimal impact on blood sugar. Aim for 2.5 to 3 cups a day. They’re packed with fiber, vitamins, and antioxidants that protect your heart and kidneys.
- Lean proteins: Fish like salmon, mackerel, and trout are rich in omega-3s, which reduce inflammation and lower heart disease risk-something people with diabetes need to watch closely. Skinless chicken, turkey, eggs, and plant-based proteins like lentils and chickpeas are also great.
- Whole grains: Swap white bread and white rice for barley, oats, quinoa, or whole-wheat pasta. These digest slower, so your blood sugar rises gently instead of crashing and spiking. A study in The Lancet showed that people who ate more whole grains had better long-term blood sugar control.
- Healthy fats: Avocados, nuts (almonds, walnuts), seeds (chia, flax), and olive oil don’t raise blood sugar. In fact, they help your body absorb nutrients and keep you full longer. A handful of almonds as a snack can prevent mid-afternoon crashes.
- Fruit: Yes, fruit is okay. Berries, apples, pears, and oranges are high in fiber and low in sugar. Avoid fruit juices-even 100% juice-because it strips away fiber and floods your system with sugar. Eat the whole fruit instead.
Foods to Avoid: The Hidden Blood Sugar Triggers
Some foods are labeled as “healthy” but are actually dangerous for diabetes. Watch out for these:- Refined grains: White bread, white rice, regular pasta, and pastries are stripped of fiber. They turn into sugar fast in your body. One slice of white bread can raise blood sugar more than a candy bar.
- Sugary drinks: Soda, sweetened tea, energy drinks, and even fruit punch are liquid sugar. A single 12-ounce can of soda has about 40 grams of sugar-that’s 10 teaspoons. That’s more than the daily limit for most adults with diabetes.
- Processed meats: Bacon, sausage, deli ham, and hot dogs are high in sodium and preservatives. Studies link them to higher insulin resistance and increased heart disease risk. Even “low-fat” versions often have added sugar to make them taste better.
- Flavored yogurts and cereals: Many “healthy” yogurts have more sugar than ice cream. Check labels. If sugar is listed as one of the first three ingredients, skip it. Choose plain, unsweetened yogurt and add your own berries.
- Added sugars: This includes honey, maple syrup, agave, and even “natural” sweeteners in packaged foods. They all behave like table sugar in your body. Baked goods, cookies, cakes, and candy are obvious, but sugar hides in sauces, salad dressings, and canned soups too.
Meal Timing Matters Just as Much as What You Eat
Eating at the same times every day helps your body predict when it needs to release insulin. Skipping meals or eating late at night can cause blood sugar swings. The American Diabetes Association recommends:- Eating every 4 to 5 hours to keep energy steady.
- Allowing 2 to 3 hours between meals so your blood sugar can drop back to a healthy range.
- Having a small, balanced snack if you’re hungry between meals-like a handful of nuts or a hard-boiled egg.
For kids with Type 2 diabetes, three small meals and three snacks a day help support growth without blood sugar spikes. Adults should aim for consistent timing too-even on weekends.
Real Meals That Work
Here are two simple, real-life meals that follow the plate method:- Southwest-Style Turkey Meatloaf: Lean ground turkey (protein), mashed red potatoes (carb), and a side of steamed green beans and a small orange (veggies and fruit). Add a drizzle of olive oil on the side.
- Easy Beef Chili: Lean beef or lentils (protein), kidney beans (carb and fiber), diced tomatoes and onions (veggies), topped with a spoonful of plain Greek yogurt. Serve with a small side salad.
These meals don’t require fancy ingredients. You can find them on the Diabetes Food Hub website, where you can build your own meal plan for free. Just drag and drop recipes into a weekly schedule.
What About Low-Carb or Keto Diets?
Some people swear by low-carb or keto diets for diabetes. While they can work for short-term weight loss and blood sugar control, they’re not for everyone. The American Diabetes Association says eating plans should be personalized. A low-carb diet might be helpful if you’re overweight and insulin resistant, but it can be hard to sustain long-term and may lack fiber and key nutrients.The Mediterranean diet, which focuses on vegetables, fish, olive oil, nuts, and whole grains, has more long-term evidence for heart health and stable blood sugar. Many people find it easier to stick with than extreme diets.

Challenges and Real-Life Solutions
Let’s be honest: eating well is harder if you’re on a tight budget, live in a food desert, or come from a culture where rice or bread is central to meals. That’s normal. The ADA estimates 23% of adults with diabetes face food insecurity. Here’s how to adapt:- On a budget: Buy frozen vegetables-they’re just as nutritious as fresh and cheaper. Canned beans (rinsed to reduce sodium) are a great protein and carb source. Eggs are one of the cheapest, most filling proteins.
- Eating out: Ask for a side of steamed veggies instead of fries. Skip the bread basket. Choose grilled over fried. Ask for sauces on the side.
- Cultural foods: You can still enjoy traditional meals. Swap white rice for brown rice or quinoa. Use less oil when cooking. Add more vegetables to stews and curries.
Why This Works Long-Term
People who stick with structured meal planning for six months or longer see HbA1c drops of 0.3% to 2.0%. That’s the difference between needing more medication and possibly reducing it. The DiRECT trial showed that some people with Type 2 diabetes even reversed their diagnosis by combining meal planning with weight loss.This isn’t about perfection. It’s about progress. One meal at a time. One plate at a time.
Can I still eat fruit if I have diabetes?
Yes, you can-and you should. Whole fruits like berries, apples, pears, and oranges are high in fiber, which slows sugar absorption. Avoid fruit juice, dried fruit, and canned fruit in syrup. Stick to one small piece or 1/2 cup of berries per serving.
Are artificial sweeteners safe for people with diabetes?
Most artificial sweeteners like stevia, sucralose, and aspartame don’t raise blood sugar. But they can still train your taste buds to crave sweetness. Some studies link them to changes in gut bacteria, which might affect insulin sensitivity over time. Use them sparingly. Water, unsweetened tea, or sparkling water with lemon are better long-term choices.
Do I need to count carbs with the plate method?
No, you don’t. The plate method is designed to replace carb counting with visual portion control. It’s simpler and works better for most people. If you’re on insulin or have trouble controlling blood sugar, your doctor or dietitian might still recommend tracking carbs-but start with the plate method first.
Can I drink alcohol with diabetes?
Moderation is key. One drink per day for women, two for men. Alcohol can cause low blood sugar, especially if you’re on insulin or certain pills. Never drink on an empty stomach. Choose dry wine, light beer, or spirits with soda water-avoid sugary mixers like tonic or juice.
What if I’m always hungry on this plan?
You’re probably not eating enough fiber or healthy fats. Add more non-starchy vegetables, nuts, seeds, avocado, or a boiled egg between meals. Drink water-sometimes thirst feels like hunger. If you’re still hungry, talk to a dietitian. You might need more protein or a slight increase in calories.
Next Steps: Start Today
You don’t need to overhaul your whole diet overnight. Pick one meal-maybe lunch-and use the plate method. Swap white rice for quinoa. Add a side of spinach. Skip the soda. Do that for a week. Then do it for dinner. Slowly, it becomes second nature.Tools like the Diabetes Food Hub, free apps from the CDC, or even a simple printed plate diagram taped to your fridge can help. If you’re unsure, ask your doctor for a referral to a certified diabetes care and education specialist. They’re trained to help you find a plan that fits your life-not the other way around.
Diabetes management isn’t about restriction. It’s about empowerment. You get to choose what fuels your body-and with the right tools, you can eat well, feel great, and stay in control.










Mukesh Pareek
The Diabetes Plate Method is fundamentally a low-glycemic load paradigm disguised as a visual heuristic. The real metabolic advantage lies in the reduction of insulinogenic amino acids and the modulation of postprandial glucagon dynamics-something most laypeople overlook. Non-starchy vegetables provide polyphenolic compounds that activate AMPK pathways, enhancing insulin sensitivity. And let’s not forget the gut microbiota shift induced by resistant starches in legumes and cooled potatoes-this isn’t just portion control, it’s epigenetic reprogramming.
Protein sources matter beyond lean vs. fatty; the leucine content in whey and eggs triggers mTOR signaling, which, in excess, may exacerbate insulin resistance over time. Hence, plant-based proteins like lentils are superior for long-term metabolic health. And olive oil? Its oleocanthal has anti-inflammatory properties comparable to ibuprofen-no wonder Mediterranean diets outperform keto in longitudinal studies.
Also, ‘small piece of fruit’ is dangerously vague. A medium apple has 25g carbs. If you’re on basal insulin, that’s a 2-unit bolus. Stop pretending this is ‘simple’-it’s a precision tool disguised as a life hack.
Saylor Frye
Wow. So you’re telling me I can’t just eat steak and avocado forever and call it ‘diabetes management’? I mean, I’ve been doing keto for 3 years and my A1c is 5.4. Why am I even reading this?
Also, ‘whole grains’? Bro, oatmeal is just sugar with fiber glued on. You’re selling a myth.
Tiffany Adjei - Opong
Oh my god, the plate method? That’s what they teach in diabetes 101? I mean, really? You’re telling me someone with prediabetes can’t just eat a salad with bacon and call it a day? No carbs? No problem.
And ‘whole grains’? Have you seen the glycemic index of quinoa? It’s 53-higher than white rice! And ‘brown rice’? That’s still a 70. You’re basically telling people to eat slower-digesting sugar. That’s not a solution, that’s a delay tactic.
Also, ‘avoid fruit juice’? What about smoothies with spinach and chia? That’s fiber-rich and delicious. You’re being so dogmatic. This is why people give up.
And don’t even get me started on ‘low-fat yogurt.’ That’s just sugar with a side of guilt. I eat full-fat Greek yogurt with stevia and berries. That’s science. Not this… this plate nonsense.
Ryan Barr
Keto works. Period.
Plate method is for people who don’t want to change.
End of story.
Cam Jane
Okay, I just want to say-this post made me cry a little. Not because it’s sad, but because I finally feel seen.
I’ve been diabetic for 12 years. I tried keto. I tried low-fat. I tried counting every carb like my life depended on it (it did). I burned out. I gained weight. I felt like a failure.
Then I tried the plate method. No apps. No scales. Just a plate. Half veggies-yes, even the weird ones I used to ignore, like bok choy and radishes. Quarter protein-I started eating eggs for breakfast again. Quarter carbs-I swapped white rice for barley. And guess what? My A1c dropped from 8.1 to 6.2 in 5 months.
And the best part? I can eat at my mom’s house now. She makes rice. I take a smaller scoop, pile on the stir-fried greens, and add grilled tofu. No one notices. I don’t feel deprived.
This isn’t about perfection. It’s about showing up. One plate at a time. You’re not failing if you eat bread once a week. You’re learning. You’re adapting. And that’s the real win.
If you’re reading this and feeling overwhelmed? Start with lunch tomorrow. Just one meal. You got this. I believe in you.
Ashley S
So you’re saying I can’t have a bagel? Or a donut? Or a slice of cake on my birthday? This is ridiculous. I’m not a robot. I have a life. You people act like diabetes is a moral failure. It’s not. It’s a condition. Eat what you want. Just take your insulin.
Why is everyone so obsessed with control? You’re not saving the world by eating quinoa. You’re just being annoying.
Leonard Shit
lol i read this whole thing and i’m just sitting here thinking… how many people actually do this? like… real people? not just the ones who have time to meal prep and a kitchen that doesn’t smell like old grease?
i work two jobs. my kid has soccer at 6. i grab whatever’s in the fridge. sometimes it’s a burrito. sometimes it’s leftover pizza. i take my metformin. i check my sugar. sometimes it’s high. sometimes it’s fine.
the plate thing sounds nice. but if i had to think about ‘quarter protein’ while my kid’s screaming for chicken nuggets… i’d just eat the nuggets and cry.
also… ‘avoid fruit juice’? bro, i drink orange juice because it’s the only thing that doesn’t make me want to vomit after my insulin shot. it’s not a lifestyle. it’s survival.
you’re not helping. you’re just making people feel worse.
Gabrielle Panchev
Wait-so you’re telling me that ‘starchy vegetables’ like sweet potatoes are okay, but white potatoes are not? But sweet potatoes are still high-glycemic, and they’re not even significantly higher in fiber than white potatoes-especially if they’re boiled, not roasted! And you say ‘whole grains’ are better, but what about sourdough? The fermentation process reduces the glycemic load dramatically-so why aren’t you recommending it? And why is ‘brown rice’ still on the list when it’s still a 68 GI? You’re being inconsistent. You’re cherry-picking studies. And you’re ignoring the fact that individual variability in glycemic response is enormous-some people spike on quinoa! Some don’t spike on white rice! This isn’t science-it’s dogma dressed up as advice.
Also, ‘one small piece of fruit’-how small? A strawberry? A grapefruit? You’re being vague on purpose. And why is ‘low-fat dairy’ recommended when fat helps slow absorption? You’re contradicting yourself. This isn’t a method-it’s a marketing brochure.
Katelyn Slack
i just wanted to say thank you for not saying ‘just lose weight’
i’ve had type 2 for 8 years. i’ve lost weight. i’ve gained it back. i’ve felt guilty every time. this post didn’t make me feel like a failure. it just gave me a way to eat without shame.
my mom is from mexico. we eat tortillas every day. i swap them for corn tortillas now. i put beans and grilled veggies on them. i don’t eat the cheese. i don’t feel like i’m giving up anything. i just… adjusted.
you don’t need to be perfect. you just need to keep going.
thank you.