When you pick up a prescription, you might not think twice about whether it’s the brand-name drug or the cheaper generic version. After all, the FDA says they’re the same. But for some people, switching from a brand-name pill to a generic one isn’t just a cost-saving move-it’s a health risk. You might feel more tired, get headaches, or notice your mood shifting. And if you’re taking a medication for thyroid disease, epilepsy, or blood thinning, those small changes can be dangerous.
What ‘the Same’ Really Means
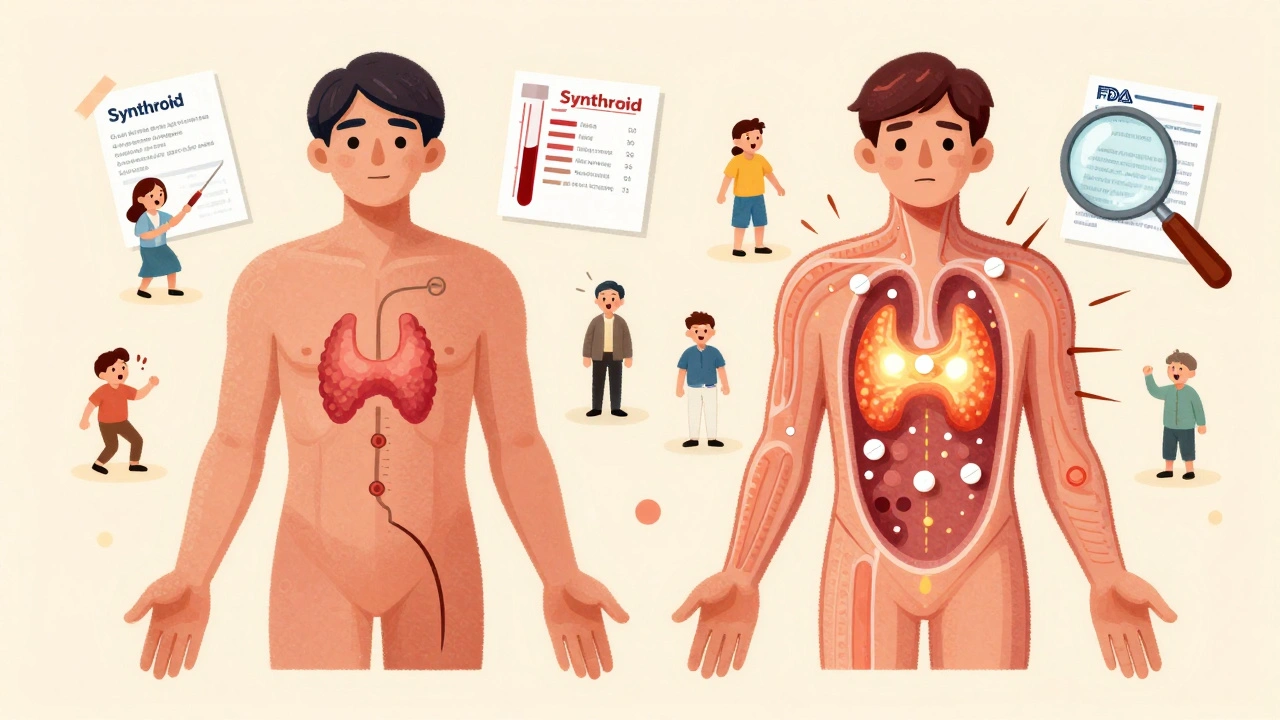
Generic drugs are required to have the same active ingredient, dose, and how they’re taken as the brand-name version. That part is true. But what’s inside the pill besides the active drug? That’s where things get messy. Generics can use different fillers, dyes, coatings, and preservatives. These are called excipients, and they make up 80% to 99% of the pill’s weight. They don’t treat your condition, but they can change how your body absorbs the medicine. The FDA allows generics to deliver between 80% and 125% of the brand-name drug’s concentration in your bloodstream. That sounds like a wide range-until you realize two different generics of the same drug can be 45% apart in how fast they’re absorbed, and both still pass FDA approval. One generic might release the drug slowly. Another might dump it all at once. For most drugs, that’s fine. For others, it’s a problem.When Small Differences Matter Most
Some medications have what’s called a narrow therapeutic index (NTI). That means the difference between a dose that works and one that’s toxic is tiny. A 10% change in blood levels can mean the difference between control and crisis. Drugs like levothyroxine (for thyroid), warfarin (a blood thinner), phenytoin (for seizures), and digoxin (for heart rhythm) fall into this category. For these, even tiny shifts in absorption can cause serious issues. A 2019 study in JAMA Internal Medicine followed over 2,000 people who switched from brand-name Synthroid to generic levothyroxine. Nearly 24% had thyroid hormone levels swing out of the safe range within six months. Only 14% of those who stayed on Synthroid had the same problem. That’s not a small difference-it’s a pattern. Patients on generic versions of lamotrigine (an epilepsy drug) saw a 17% spike in breakthrough seizures after switching, compared to just under 9% for those who stayed on the brand. Meanwhile, for drugs like metformin (for diabetes), studies show no real difference. The issue isn’t generics as a whole-it’s which generic you’re taking, and what you’re taking it for.What Patients Are Reporting
Real people are noticing this. On Drugs.com, nearly 4 out of 10 people taking generic levothyroxine said they felt worse than when they were on the brand. Common complaints? Fatigue, mood swings, brain fog. On Reddit’s r/pharmacy, over 60% of users who switched to generic bupropion (an antidepressant) reported new or worse side effects-headaches, anxiety, insomnia. Pharmacists are seeing it too. A 2022 survey of over 3,200 community pharmacists found that 68% had patients come in with new symptoms after switching generics. More than 40% said it happened frequently-five or more times a month. One thyroid patient group surveyed nearly 5,000 people. Over 70% said their symptoms got worse after switching to generic levothyroxine. More than half needed their dose adjusted just to feel normal again.
Why This Isn’t Just ‘In Their Head’
Some doctors say these reactions are placebo effects. Maybe the patient expects to feel worse, so they do. But the data doesn’t back that up. The same people who feel fine on one generic version get sick when switched to another-same drug, same dose, different manufacturer. That’s not psychology. That’s pharmacology. A 2019 study in the New England Journal of Medicine found that 28% of people on complex medication regimens had adverse effects when switched between different generic versions of the same drug. Only 12% had issues when they stayed on the same formulation. The switch itself was the trigger. And it’s not just about absorption. Some generics use excipients like bisulfites, which can trigger asthma attacks in 5-10% of asthmatic patients. If you’re allergic to sulfites and your new generic contains them, you’re not imagining the wheezing-you’re reacting to a chemical you didn’t know was in your pill.What You Can Do
If you’re on a medication with a narrow therapeutic index, don’t assume all generics are safe swaps. Here’s what works:- Ask your doctor to write ‘Do Not Substitute’ on your prescription. That stops the pharmacy from switching you without approval.
- Stick with one generic manufacturer. If you start on a generic, keep taking the same brand of generic. Don’t let your pharmacy swap it out.
- Track your symptoms. Keep a simple log: date, dose, how you feel, any new side effects. This helps your doctor spot patterns.
- Check inactive ingredients. The FDA has a public database of all inactive ingredients in approved drugs. Ask your pharmacist for the exact formulation you’re taking.
- Get blood tests. If you’re on levothyroxine, warfarin, or phenytoin, ask for a follow-up test 4-6 weeks after any switch. TSH, INR, or drug levels can tell you if the new version is working.
The Bigger Picture
The FDA says 99.7% of generics meet bioequivalence standards. That’s true. But standards are set for populations, not individuals. What’s safe for 99 out of 100 people might not be safe for you. The European Union uses tighter standards for NTI drugs-90% to 111% absorption range-instead of the FDA’s 80%-125%. As a result, fewer generics are approved in Europe for these drugs, but patient outcomes are more consistent. In 2023, the FDA approved the first ‘authorized generic’ of Synthroid. That’s the exact same pill as the brand, just sold under a different name and at a lower price. It’s a step toward solving this problem without sacrificing cost savings. Research is also moving toward personalized medicine. A 2024 study showed that genetic testing can predict how someone will respond to certain generics with over 80% accuracy. In the future, your DNA might tell your doctor which version of a drug is safest for you.It’s Not About Trusting Generics-It’s About Choosing Wisely
Generics saved the U.S. healthcare system $373 billion in 2022. That’s huge. For most people, generics are safe, effective, and life-changing. But for a small group-people on NTI drugs, those with allergies, or those who’ve had bad reactions before-switching isn’t a simple swap. It’s a medical decision. And you have the right to control it. If you’ve ever felt off after a pharmacy switch, you’re not alone. And you’re not crazy. Your body might just be telling you that not all ‘the same’ drugs are created equal.Are generic medications always as safe as brand-name drugs?
For most medications, yes. Generics are required to meet strict FDA standards for active ingredients and absorption. But for drugs with a narrow therapeutic index-like levothyroxine, warfarin, or phenytoin-even small differences in how the body absorbs the drug can cause serious side effects. In these cases, switching between generics or from brand to generic can lead to measurable changes in blood levels and symptoms.
Why do some people feel worse on generic levothyroxine?
Levothyroxine has a very narrow therapeutic window-tiny changes in blood levels affect how your thyroid functions. Different generic versions may absorb slightly differently due to variations in inactive ingredients or manufacturing. Studies show nearly 24% of patients switching to generic levothyroxine experience thyroid hormone levels that go out of the safe range, leading to fatigue, weight changes, or mood swings. Many need their dose readjusted after the switch.
Can excipients in generics cause side effects?
Yes. While inactive ingredients don’t treat your condition, they can cause reactions. For example, some generics use bisulfites as preservatives, which can trigger asthma attacks in 5-10% of asthmatic patients. Others contain dyes or fillers that cause headaches, rashes, or digestive upset in sensitive individuals. You can check the exact ingredients using the FDA’s Inactive Ingredient Database.
Should I avoid generic medications entirely?
No. Generics are safe and effective for the vast majority of drugs and patients. For conditions like high blood pressure, diabetes (except insulin), or cholesterol, switching to generics rarely causes issues. But if you’re on a medication with a narrow therapeutic index-or if you’ve had a bad reaction after a switch-ask your doctor to specify ‘Do Not Substitute’ on your prescription and stick with one consistent version.
How can I find out which generic manufacturer I’m getting?
Ask your pharmacist. The name of the manufacturer is usually printed on the bottle or the label. You can also request the FDA’s Inactive Ingredient Database to look up the exact formulation. Keeping a record of which manufacturer you’re on helps you spot patterns if side effects appear after a switch.
What should I do if I think my generic medication isn’t working?
Don’t stop taking it. Contact your doctor and pharmacist immediately. Keep a symptom log-note when you switched, what symptoms started, and how severe they are. Ask for a blood test if you’re on a narrow therapeutic index drug (like TSH for thyroid or INR for warfarin). You may need to switch back to your previous version or request a brand-name drug if it’s medically necessary.









Steve Sullivan
so like... if your body's got a weird reaction to a pill, it's not 'in your head' - it's your body going 'hey, this filler smells like regret'.
generic levothyroxine? i switched once. felt like a zombie who forgot how to breathe. went back to brand. instant human again.
why are we okay with this? we don't swap engine parts in our cars and call it 'the same'.
pharma companies aren't evil, but they're not saints either. they're playing the system. and we're the guinea pigs.
ask for the manufacturer name. write it down. stick to it. your thyroid will thank you.
also - check the inactive ingredients. if you're allergic to sulfites and your pill has bisulfites? yeah. that's not a coincidence.
the FDA says 'close enough'. but your body? it knows the difference.
Evelyn Pastrana
my mom switched to generic warfarin and started bleeding out of her nose at 3am. we thought it was a cold. turned out her INR was 8.8. 8.8. 😳
now she gets the same generic, every time. no substitutions. doctor wrote 'do not substitute' in like, 14-point bold.
also - she keeps a little notebook. 'day 3: headache. day 5: dizzy. day 7: back to normal'. it's weirdly romantic.
Sarah Gray
Of course the FDA says generics are fine - they’re regulated by the same people who approved thalidomide and Vioxx. Trust the system? Please. You’re one blood test away from a thyroid crisis.
And don’t even get me started on how they let companies use the same generic name for three different formulations. It’s a fucking lottery.
People who say 'it’s all placebo' haven't been on a narrow therapeutic index drug. Or they’re on the payroll.
I’ve seen patients cry because they lost their job after switching to a generic that made them too tired to drive. And the doctor just shrugged and said, 'Maybe you need more coffee.'
It’s not just pharmacology. It’s negligence dressed up as savings.
Michael Robinson
if you’re on a pill that’s got a tiny window between 'works' and 'kills you', then yeah - small changes matter.
it’s like driving a car with a gas pedal that sometimes presses 10% harder. you don’t want that.
the system’s not broken. it’s just lazy. it’s built for masses, not people.
we need better rules for the drugs that matter most.
Kathy Haverly
Oh, so now we’re blaming the generics? Let me guess - you also think the moon landing was fake and your coffee is secretly laced with fluoride.
Everyone who says they 'feel worse' on generics is just anxious. You don’t like change. You don’t like being told you’re not special.
And your 'symptom log'? Cute. I bet you color-code it.
Meanwhile, millions of people take generics and don’t turn into zombies. Maybe your problem isn’t the pill - it’s your brain.
Andrea Petrov
Did you know the FDA doesn’t test generics themselves? They just review the manufacturer’s data. And guess who pays for that data? The manufacturer.
So if your generic is made by a company that bribes the reviewer? You’re not getting 'bioequivalent' - you’re getting a placebo with a fancy label.
And don’t even mention the 'authorized generic' of Synthroid - that’s just the brand repackaged. The real generics? Still a gamble.
They’re hiding this from us. Why? Because if people knew, they’d stop buying generics. And then the profits drop.
I’ve seen the emails. I’ve seen the redactions.
Suzanne Johnston
It’s fascinating how we treat medicine like a commodity - interchangeable, mass-produced, disposable.
But the human body isn’t a factory line. It’s a symphony. And sometimes, a single wrong note - even a slightly different coating on a pill - can throw the whole thing off.
Maybe the real problem isn’t generics. It’s our belief that everything can be standardized. Even when it shouldn’t be.
We need to stop treating people like data points and start treating them like... people.
Graham Abbas
I once had a friend who switched from brand to generic lamotrigine and had a seizure during a wedding. A WEDDING. The bride cried. The groom panicked. The generic? 'Made in India, batch #X789.'
He’s back on brand now. Costs $400 a month. Worth every penny.
And the pharmacy? They didn’t even call to ask if he was okay. Just shipped the next bottle.
Medicine isn’t cereal. You don’t just swap flavors and hope for the best.
Haley P Law
so i switched to generic levothyroxine and felt like my soul was being slowly drained by a fax machine 🤖
my therapist said 'it’s probably anxiety' 😭
i switched back. 3 days later i cried because the sun felt warm on my face again. like, for the first time in months.
doctors need to stop talking like we’re robots with a 'medication update' button.
Andrea DeWinter
if you're on levothyroxine or warfarin - don't just take whatever the pharmacy gives you.
ask for the manufacturer name. write it down. keep it.
if you switch and feel off - get a blood test. don't wait. don't hope it gets better.
your doctor doesn't know what pill you got unless you tell them.
be your own advocate. it's not rude - it's survival.
Chris Marel
i come from a place where people can't afford brand drugs. but i’ve seen someone die because they couldn't get the right generic.
this isn't about being rich or poor. it's about access to safe medicine.
if the system fails people like my aunt - who took her thyroid med for 15 years and then switched and had a stroke - we need to fix it.
not blame her. not call her dramatic.
fix the system.
ian septian
stick to one generic. track your symptoms. ask for blood tests.
done.
Morgan Tait
you know what’s wild? the same company that makes the brand-name Synthroid also makes the 'generic' version - just under a different name and with a cheaper label.
so when they say 'generic', sometimes they mean 'the same pill, but you’re paying less because you’re dumb enough to believe it’s different.'
and the FDA? They’re fine with it.
Meanwhile, your pharmacist has no idea which version you’re getting - they just grab the cheapest one off the shelf.
it’s not conspiracy. it’s capitalism.
if you want to stay alive? Don’t let a warehouse worker choose your medicine.
ask for the name on the bottle. write it down. scream it if you have to.
they don’t care. but you? you have to care enough to fight.
Darcie Streeter-Oxland
It is, regrettably, an incontrovertible fact that the regulatory framework governing pharmaceutical equivalence is predicated upon population-level metrics, thereby rendering it inherently insufficient for the management of individualized therapeutic responses.
Furthermore, the utilization of excipients with known allergenic potential, without mandatory disclosure in standardized packaging, constitutes a significant breach of patient autonomy.
It is imperative that clinicians be mandated to engage in informed consent procedures prior to any substitution of prescribed medication.
One might reasonably posit that the current paradigm prioritizes fiscal efficiency over clinical fidelity - a morally indefensible compromise.
Taya Rtichsheva
so i switched to generic bupropion and suddenly i was screaming at my cat for breathing too loud 😭
then i switched back and i cried because my cat looked at me like 'hey, you’re back'
pharmacies are like that one friend who swaps your coffee creamer without asking
and then you’re like... why does this taste like betrayal
Christian Landry
my cousin had a seizure after switching generics - and the pharmacist didn’t even know the difference between the two versions.
we asked for the manufacturer name on the bottle - they said 'oh, we just get whatever’s cheapest.'
how is that okay?
if you’re on a high-risk med, ask for the exact name. write it down. show your doctor.
also - the FDA database is free. you can look up every ingredient. it’s not hard.
we’re not asking for luxury. just safety.
❤️
Katie Harrison
I appreciate the depth of this post - truly. But I want to gently remind everyone: not all generics are created equal, and not all patients are the same.
As someone who has lived with hypothyroidism for over two decades, I’ve tried five different generics. Only two felt tolerable. One made me feel like I was underwater. Another made me weep for no reason.
My advice? Don’t just accept the first version you’re given. Try one. Wait six weeks. Test. If it’s off - speak up. Document. Switch back.
Your health is not a cost-saving metric.
It’s yours.
Mona Schmidt
Many people assume that because two drugs contain the same active ingredient, they are functionally identical. This is a dangerous misconception.
The bioavailability of a drug is influenced by numerous factors: particle size, crystalline form, dissolution rate, and yes - even the type of coating used.
For medications with a narrow therapeutic index, these differences are not trivial. They are clinically significant.
Furthermore, regulatory agencies in the United States allow a 20% variance in absorption - a range that is simply too wide for drugs like warfarin or phenytoin.
The European Union’s stricter standards (90–111%) are not just conservative - they are scientifically superior.
We must advocate for policy change that prioritizes patient safety over corporate profit margins.
This is not anti-generic. It is pro-safety.
Guylaine Lapointe
Oh great. Another article telling us the system is rigged. Newsflash: it is. And guess what? Nothing will change until people stop being polite about it.
You think your doctor cares that your thyroid levels are off? No. They care that the insurance company approved the cheaper pill.
And you? You’re supposed to be grateful you got anything at all.
So here’s my take: if you’re on a critical med, demand the brand. If they say no, escalate. Call your state medical board. File a complaint. Tweet it. Make noise.
They’ll ignore you until you become a problem.
Be the problem.
Steve Sullivan
my mom switched to a different generic of levothyroxine last year. same dose. same pharmacy. different manufacturer.
she started forgetting her own birthday.
we switched back. she remembered her cat’s name again.
the pharmacy didn’t even tell us they changed it.
so now i call them every time. 'what manufacturer is this?' they hate me.
good.