Most people know that mixing two pills can cause problems. But what if your health condition makes a perfectly safe drug dangerous? This isn’t theory-it’s happening right now in homes, clinics, and hospitals. A person with heart failure takes ibuprofen for a headache and ends up back in the hospital. Someone with diabetes uses a beta-blocker for high blood pressure and misses the warning signs of low blood sugar. These aren’t mistakes-they’re drug-disease interactions, where a medication meant to help one condition makes another one worse.
What Exactly Is a Drug-Disease Interaction?
A drug-disease interaction (also called a drug-condition interaction) happens when a medicine used to treat one illness harms another condition you already have. It’s not about pills clashing with each other-that’s a drug-drug interaction. This is about how your body’s existing problems change how a drug works. For example, if you have kidney disease, your body can’t clear certain drugs like metformin properly. That leads to a dangerous buildup of lactic acid. Or if you have asthma, beta-blockers meant to lower your blood pressure can tighten your airways and trigger an attack. These interactions are silent killers. They don’t always show up on lab tests. You might feel fine-until you suddenly don’t. The Agency for Healthcare Research and Quality estimates that 5-10% of hospital admissions are caused by medication problems, and many of those come from unnoticed drug-disease clashes.How Do These Interactions Happen?
There are five main ways your health condition changes how a drug behaves in your body:- Pharmacodynamic interference: The drug’s effect fights against your disease. Beta-blockers reduce heart rate, which helps high blood pressure-but they also hide the shaking, sweating, and fast heartbeat that warn you your blood sugar is dropping. For someone with diabetes, that’s a recipe for a dangerous low.
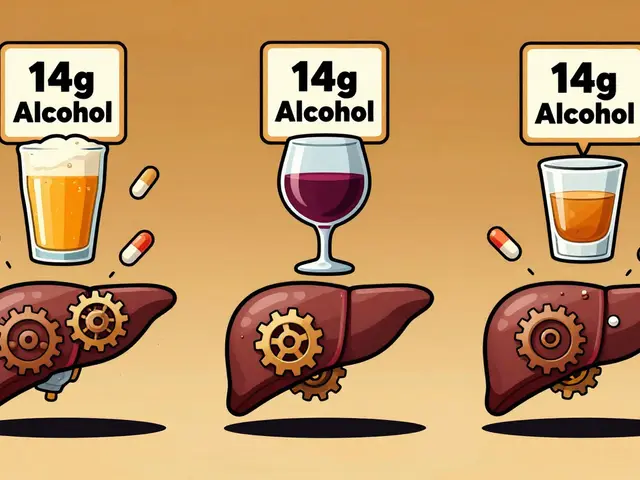
- Pharmacokinetic changes: Your disease changes how your body absorbs, breaks down, or gets rid of the drug. Liver disease slows down how fast warfarin is processed. That means the same dose can become toxic. Kidney failure stops metformin from leaving your system, leading to lactic acidosis.
- Masking symptoms: The drug hides signs of a worsening condition. Diuretics for heart failure can make you feel better by reducing swelling-but they also lower potassium, which can trigger dangerous heart rhythms you won’t notice until it’s too late.
- Exacerbating complications: The drug makes your condition worse. NSAIDs like naproxen cause your body to hold onto salt and water. That’s fine for a healthy person. But if you have heart failure, that extra fluid pushes your heart harder and can send you into acute failure.
- Direct organ toxicity: The drug damages an organ already weakened by disease. Certain antibiotics can harm kidneys already struggling from diabetes or high blood pressure.
High-Risk Conditions and Common Culprits
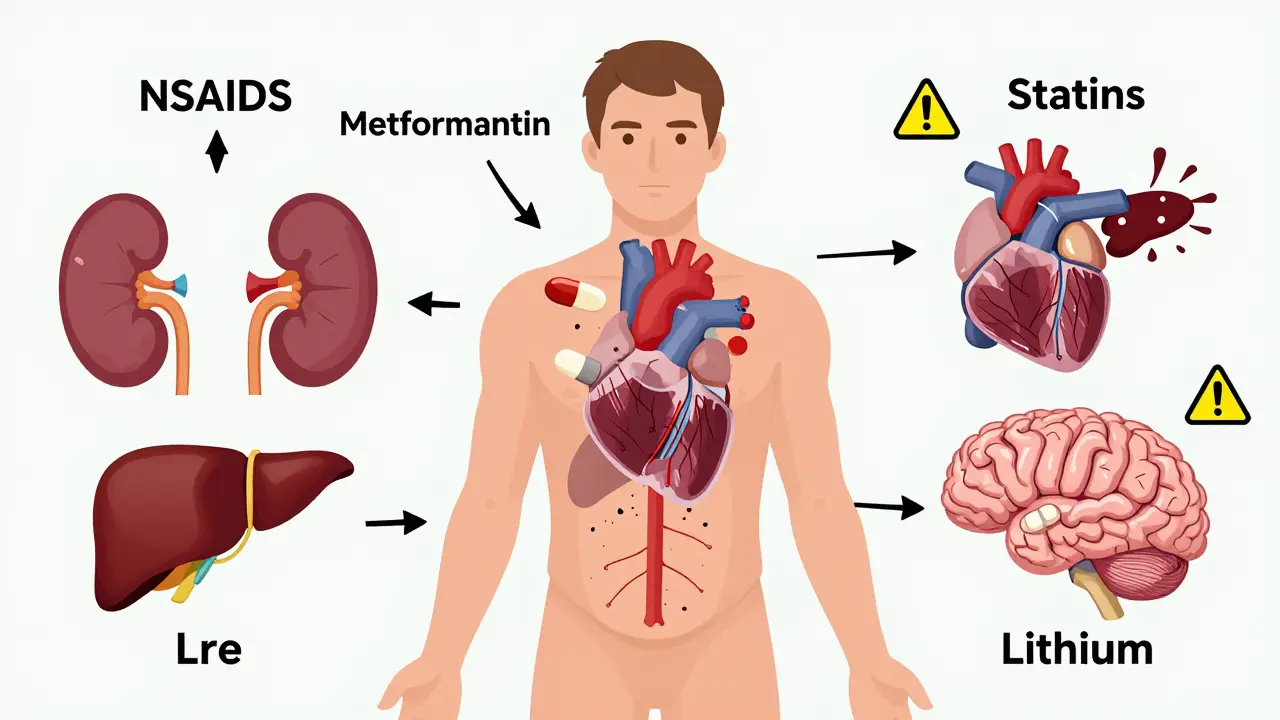
Some health problems are especially dangerous when paired with common medications. The top four are kidney disease, heart failure, liver disease, and psychiatric conditions. Together, they account for nearly 80% of serious drug-disease interactions.Chronic Kidney Disease: Over 80% of dangerous interactions in diabetes guidelines involve kidney problems. Drugs like metformin, NSAIDs, and contrast dyes used in imaging scans can all cause acute kidney injury or lactic acidosis. Even common painkillers like ibuprofen can reduce blood flow to the kidneys, making things worse.
Heart Failure: NSAIDs are the biggest offender here. They cause fluid retention and raise blood pressure, both of which strain the heart. Beta-blockers can help heart failure-but if the dose is too high or the patient has severe disease, they can drop blood pressure too far. Digoxin and lithium levels also rise dangerously in heart failure patients because their kidneys can’t clear them.
Liver Disease: The liver breaks down most drugs. If it’s damaged by hepatitis, alcohol, or fatty liver disease, drugs like statins, opioids, and benzodiazepines build up in the blood. That leads to excessive drowsiness, confusion, or even coma. Even over-the-counter supplements like St. John’s wort can cause serotonin syndrome when mixed with antidepressants.
Psychiatric Conditions: Antidepressants like SSRIs increase bleeding risk, especially in people with liver disease or those taking blood thinners. Lithium, used for bipolar disorder, becomes toxic if kidney function drops-even slightly. And antipsychotics can cause dangerous drops in blood pressure or abnormal heart rhythms in patients with existing heart conditions.

Why Are These Interactions So Often Missed?
You’d think doctors would catch this. But they don’t always. Here’s why:- Guidelines ignore comorbidities: Most treatment guidelines focus on one disease at a time. A diabetes guideline tells you how to control blood sugar-but rarely warns that metformin is risky if you also have kidney disease. A heart failure guideline might say to avoid NSAIDs-but not mention that some beta-blockers can mask hypoglycemia in diabetic patients.
- EHR alerts are noisy: Electronic health records flag drug-disease interactions, but they’re wrong nearly half the time. That means doctors start ignoring them. If you get 10 alerts a day and 8 are useless, you stop looking.
- Time is short: A community pharmacist spends about 13 minutes per patient checking for interactions. That’s not enough when someone is on six different meds and has four chronic conditions.
- Patient education is weak: Only 22% of people with high blood pressure know why decongestants like pseudoephedrine can spike their pressure. Most patients don’t realize that a cold medicine can undo their heart treatment.
What Can You Do?
You don’t have to wait for your doctor to catch it. Here’s what works:- Keep a full medication list: Include prescriptions, over-the-counter drugs, supplements, and even herbal teas. Bring it to every appointment. Write down why you take each one.
- Ask the right questions: When a new drug is prescribed, ask: “Could this make any of my other conditions worse?” or “Is this safe with my kidney/liver/heart problem?”
- Use the Beers Criteria: This is a trusted list of medications that are risky for older adults with common conditions. You can find it online or ask your pharmacist for a copy.
- Monitor your symptoms: If you start feeling worse after starting a new drug-fatigue, swelling, confusion, dizziness, irregular heartbeat-don’t assume it’s just aging. Call your provider.
- Get a medication review: Many pharmacies offer free reviews. A pharmacist can look at your whole list and spot hidden risks you didn’t know about.
What’s Changing in Medicine?
The tide is turning. The FDA now requires drug makers to test their medicines in patients with common comorbidities-not just healthy volunteers. The European Medicines Agency demands a dedicated section in every new drug’s label about disease interactions. The NIH’s All of Us program is using AI and genetic data to predict who’s at highest risk. Early results show 38% better accuracy than old methods.Machine learning tools are now predicting dangerous interactions with 89% accuracy by analyzing 157 factors-from lab values to age to other meds. Mayo Clinic’s DDSI screening program cut readmissions by 27%. These aren’t futuristic ideas-they’re happening now.
But progress is uneven. Medical schools teach an average of just 4.2 hours on drug-disease interactions. Only 31% of clinical guidelines include comorbidity warnings. And marginalized communities face 23% higher rates of harm because their care is fragmented and rushed.
Bottom Line
Medications aren’t one-size-fits-all. What helps one person can hurt another-not because of the drug, but because of the person. Your health conditions change how your body handles medicine. Ignoring that is like giving a life jacket to someone who can’t swim and assuming it’ll work the same for everyone.The solution isn’t more drugs. It’s better thinking. Ask questions. Know your conditions. Speak up. And if your doctor doesn’t consider how your heart, kidneys, liver, or mental health affect your meds, find one who does. Your life might depend on it.
Can a drug that’s safe for most people be dangerous for me?
Yes. A drug that’s perfectly safe for someone with no other health issues can be harmful if you have kidney disease, heart failure, liver problems, or certain mental health conditions. For example, metformin is a common diabetes drug, but it can cause lactic acidosis in people with reduced kidney function. Beta-blockers help high blood pressure but can hide signs of low blood sugar in diabetics. Safety depends on your full health picture, not just the condition being treated.
Are over-the-counter medicines safe if I have chronic conditions?
Not always. Many people assume OTC drugs are harmless, but that’s not true. NSAIDs like ibuprofen or naproxen can worsen heart failure and kidney disease. Decongestants like pseudoephedrine can spike blood pressure in people with hypertension. Even antacids can interfere with kidney function or cause electrolyte imbalances. Always check with your pharmacist before taking any OTC medicine if you have chronic health issues.
How do I know if a new medication is causing a drug-disease interaction?
Watch for new or worsening symptoms after starting a new drug. Signs include sudden swelling, extreme fatigue, confusion, irregular heartbeat, dizziness, or unexplained changes in urination. If you notice any of these, don’t ignore them. Write down when the symptom started and what medication you began around that time. Bring this to your provider-they may need to adjust your treatment.
Do pharmacists check for drug-disease interactions?
Many do, but not always during a quick refill. Community pharmacists are trained to spot these interactions, but they often don’t have enough time during routine dispensing. Ask for a medication therapy review-many pharmacies offer this for free. It’s a 20-30 minute session where the pharmacist reviews all your meds, conditions, and supplements to find hidden risks. Don’t wait until you’re in the hospital to ask.
Why don’t doctors always warn me about these interactions?
Many clinical guidelines focus on treating one disease at a time, not how multiple conditions interact. Also, electronic alerts in hospital systems are often inaccurate, leading doctors to ignore them. Time pressure, lack of training, and outdated protocols mean drug-disease interactions are still under-recognized. It’s not negligence-it’s a system flaw. That’s why you need to be your own advocate. Ask questions. Bring your full list of meds and conditions to every appointment.









Shawn Peck
This whole post is just common sense, but nobody wants to admit it. Ibuprofen for heart failure? That’s like putting a bandaid on a gunshot wound. And don’t even get me started on metformin with bad kidneys-people think ‘natural’ means safe, but your body ain’t a fucking fairy tale. Stop blaming doctors. Start reading the damn label.
Sarah Blevins
While the article presents a compelling narrative regarding pharmacodynamic and pharmacokinetic interactions, it lacks quantitative granularity in its statistical claims. The assertion that ‘5–10% of hospital admissions are caused by medication problems’ is cited without primary source attribution. Furthermore, the Beers Criteria reference is appropriately contextualized, yet no distinction is made between guideline recommendations and evidence-based thresholds for clinical intervention. A more rigorous framing would enhance its utility in clinical decision-making.
Jason Xin
Yeah, I’ve seen this too many times. My grandma was on lisinopril and ibuprofen for ‘a little arthritis pain.’ She didn’t even know the NSAID was killing her kidneys. Took three months for anyone to catch it. Pharmacists are the real heroes here-they’re the ones who actually look at your whole list, not just one prescription at a time. If your doc doesn’t ask about your OTC stuff, they’re not doing their job. And yeah, I’m being sarcastic about how ‘everyone knows’ this stuff. They don’t. And that’s scary.
Yanaton Whittaker
AMERICA IS BEING POISONED BY BIG PHARMA AND LIBERAL MEDICAL GUIDELINES! 💥 They don’t want you to know that NSAIDs are a communist plot to weaken the American heart! I’ve been taking aspirin since 1987 and I’m 78 and still running marathons! Your doctor’s EHR is just a surveillance tool to make you dependent on pills! #DrugsAreTheEnemy #FreeMyKidneys 🇺🇸🔥
Kathleen Riley
The ontological framework underpinning the discourse on drug-disease interactions reveals a fundamental epistemological deficit within contemporary medical paradigms: the reification of pharmaceutical agents as discrete, context-agnostic entities, rather than as dynamic, phenomenologically embedded interventions within the lived organism. The clinical imperative, therefore, transcends pharmacological reductionism and demands a hermeneutic approach to therapeutics-one that situates the patient not as a vector of pathology, but as a singular, embodied narrative of physiological complexity.
Beth Cooper
Okay but have you heard about the 2017 WHO memo that got buried? They found that drug-disease interactions are actually caused by 5G towers messing with your liver enzymes. The FDA knows this. That’s why they push beta-blockers-they’re part of the mind-control program. I took a cold medicine once and my blood sugar went nuts. Coincidence? Nah. They want us sick so we keep buying pills. Also, your pharmacist is probably a robot. I saw one blink. 😏
Donna Fleetwood
You know what? This is exactly why I started keeping my med list on my phone and bringing it to every appointment-even the dermatologist. I used to think ‘I’m fine, I don’t need to say anything.’ But after my mom almost went into heart failure from an OTC decongestant, I learned: speak up, even if it feels awkward. You’re not being difficult-you’re saving your life. And hey, if your doc rolls their eyes? Find a new one. You deserve better. 💪❤️
Shubham Dixit
Listen, in India we don’t have all these fancy EHR systems, but we know this stuff by heart. My uncle had diabetes and kidney disease-he took ibuprofen for back pain, and within two weeks he was in dialysis. The pharmacist there, old man with spectacles and a chai cup, looked at his list and said, ‘Beta, this is not medicine, this is poison.’ We don’t need AI to tell us that. We’ve been surviving this since before your hospitals were built. The real problem? You think technology fixes everything. No. It’s wisdom, not algorithms. And you Americans think you’re so advanced-you’re just drowning in pills and alerts. We don’t need your 89% accuracy. We need respect for the body. And stop calling it ‘drug-disease interaction’-it’s just common sense. Why do you need a PhD to understand that bad kidneys can’t handle bad drugs? We knew that in 1970.
KATHRYN JOHNSON
Stop. Just stop. This is why people die.