Cirrhosis Treatment: What Works, What Doesn’t, and What You Need to Know
When your liver gets scarred from long-term damage, it’s called cirrhosis, a late-stage liver disease where healthy tissue is replaced by scar tissue, impairing function. Also known as liver cirrhosis, it doesn’t reverse—but stopping further damage is possible, and sometimes life-saving. This isn’t just about quitting alcohol. Cirrhosis can come from fatty liver disease, hepatitis, autoimmune conditions, or even long-term medication use. The key is catching it early and acting fast.
Alcoholic liver disease, a leading cause of cirrhosis, responds dramatically to complete abstinence. Studies show that people who stop drinking before advanced scarring sets in can stabilize their condition for years. Nonalcoholic fatty liver disease, often tied to obesity and diabetes, improves with weight loss and blood sugar control. Losing just 5–10% of body weight can reduce liver fat and inflammation. Medications like pioglitazone or vitamin E help in some cases, but they’re not magic pills—lifestyle is the real treatment.
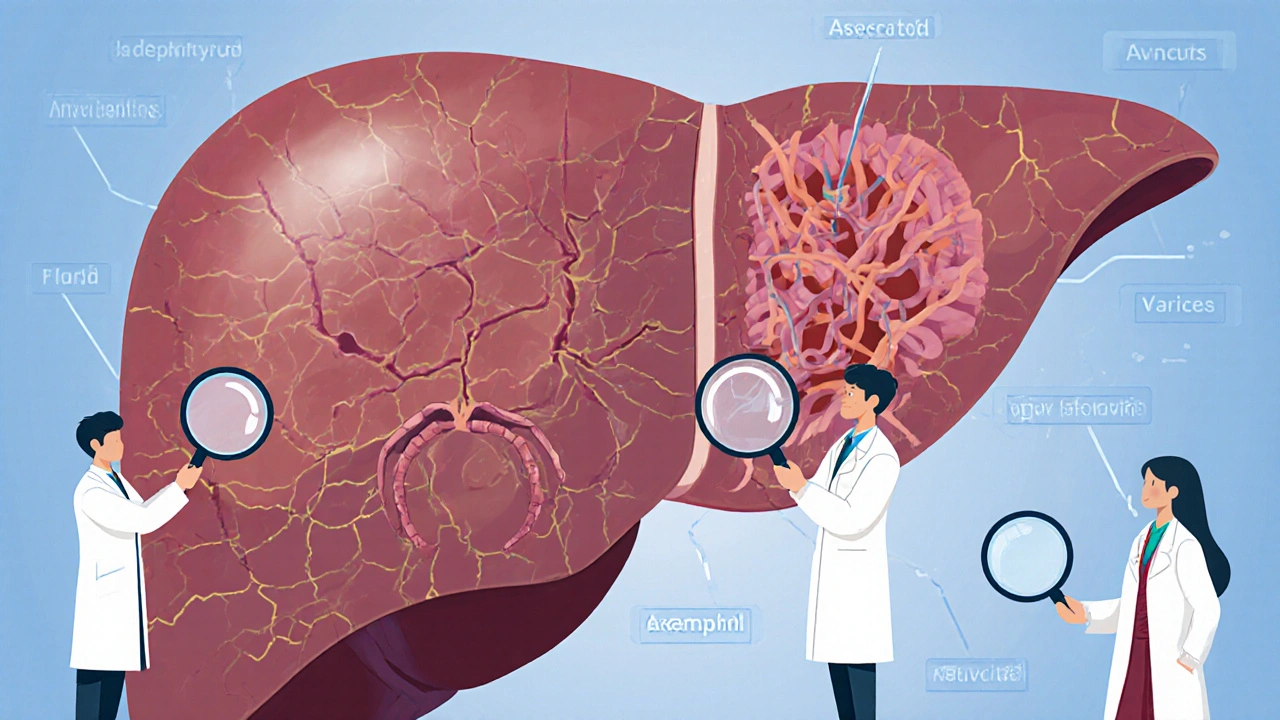
Not all cirrhosis is caused by lifestyle. Hepatitis C, a viral infection that attacks the liver, can now be cured in most cases with 8–12 weeks of antiviral pills. If you’ve had cirrhosis from hepatitis C and get treated early, your liver can actually heal a bit. But if the scarring is too far along, the virus won’t be the main problem anymore—it’s the complications: fluid buildup, bleeding, confusion, or liver cancer. That’s when you need specialists, not just general advice.
Some people hear "cirrhosis" and think it’s a death sentence. It’s not. Many live for decades with it if they manage it right. The goal isn’t to reverse the scars—it’s to stop them from spreading. That means avoiding alcohol, checking every supplement you take (some herbs wreck the liver), watching your salt intake, and getting regular scans for liver cancer. Your doctor should monitor your platelets, albumin, and bilirubin levels. These numbers tell you if your liver is holding on or slipping.
When things get serious, liver transplant, the only cure for end-stage cirrhosis, becomes the focus. It’s not easy—waiting lists are long, and you have to prove you’re sober and committed to lifelong care. But for those who qualify, it’s life-changing. People come out of transplant with energy they haven’t had in years. But transplant isn’t the only path. For many, the best treatment is the one they start today: eating better, moving more, skipping alcohol, and listening to their liver before it screams.
Below, you’ll find real-world guides on how medications, diet, and monitoring play into managing liver damage. Some posts talk about drug interactions that hurt the liver. Others show how to spot early warning signs before cirrhosis hits. These aren’t theoretical—they’re from people who’ve been there. And if you’re reading this, you’re already ahead of the game.
Cirrhosis is the advanced stage of chronic liver disease, marked by scarring and declining function. Learn about its major complications-ascites, bleeding, brain fog, and cancer-and how to manage them with diet, meds, and monitoring.