Heart disease isn’t just something that happens to older people. It’s a silent process that builds over years, often without warning. And while it’s true that some risk factors like age and family history are out of your control, the biggest killers - the ones that actually cause most heart attacks - are completely preventable. The heart disease risk factors you can change are the ones that matter most right now.
Age: Time Is a Silent Factor
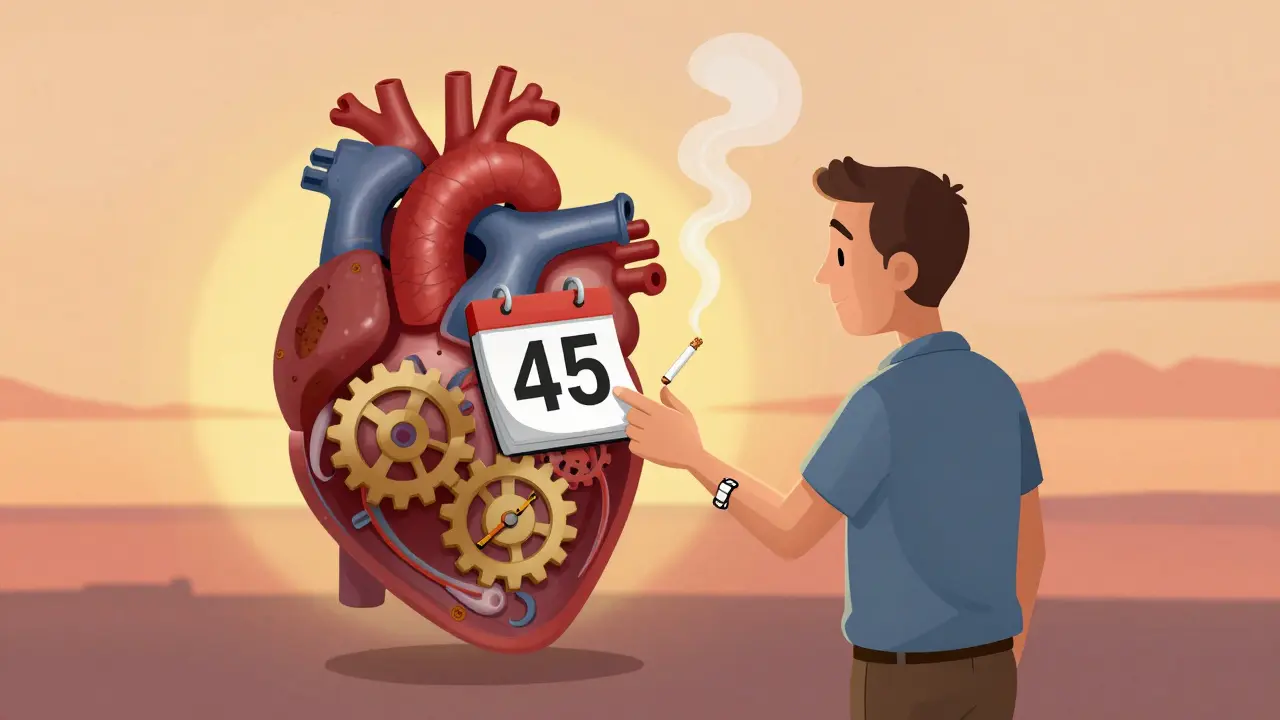
You can’t turn back the clock, but you can understand how time affects your heart. For men, risk starts climbing noticeably after 45. For women, it’s after 55. That’s not a magic number - it’s when hormonal changes, especially after menopause, start to shift how your body handles cholesterol and blood pressure. By age 70, your lifetime chance of developing heart disease jumps to about 70% for men and 60% for women. Each decade adds roughly 10% more risk, independent of everything else. This isn’t about getting old - it’s about what decades of lifestyle choices do to your arteries. Even if you’re young, knowing this helps you act early.Family History: Your Genetic Blueprint
If a parent or sibling had a heart attack or needed a stent before age 55 (for men) or 65 (for women), your risk goes up by 60% to 75%. That’s not a guess - it’s from the INTERHEART study, one of the largest ever done on heart disease. Some people inherit a condition called familial hypercholesterolemia, which affects 1 in 250 people globally. Left untreated, it can raise heart attack risk by 13 to 20 times. You might not know you have it until you have a heart attack. That’s why knowing your family history isn’t just about guilt - it’s about getting tested. A simple cholesterol panel can catch it early. And if your dad had a heart attack at 48? You need to be proactive, not hopeful.Smoking: The Single Biggest Preventable Killer
Smoking isn’t just bad for your lungs. It’s a direct attack on your heart. Current smokers have two to four times the risk of coronary heart disease compared to people who’ve never smoked. Even light smoking - just one to five cigarettes a day - increases your risk by 50%. That’s not a typo. A 2020 study in JAMA Internal Medicine found that smoking this little still damages your blood vessels, raises blood pressure, and makes your blood more likely to clot. In the U.S., smoking causes about 1 in every 4 cardiovascular deaths. But here’s the good news: quit today, and within one year, your risk drops by half. After 15 years, it’s nearly the same as someone who never smoked. Quitting isn’t about willpower alone - it’s about removing the most powerful toxin your heart has to deal with.High Blood Pressure: The Silent Saboteur
You can’t feel high blood pressure. That’s why it’s called the silent killer. Nearly half of American adults have it - that’s 116 million people. But most don’t know it. Uncontrolled, it increases your heart disease risk by 300% to 400%. The SPRINT trial showed that lowering systolic pressure to below 120 mmHg (instead of the old 140 target) cuts cardiovascular events by 25%. That’s huge. It doesn’t mean you need medication right away. But if your reading is 130/80 or higher, you’re already in the danger zone. Start tracking it at home. Cut back on salt. Move more. Sleep better. These aren’t suggestions - they’re your first line of defense.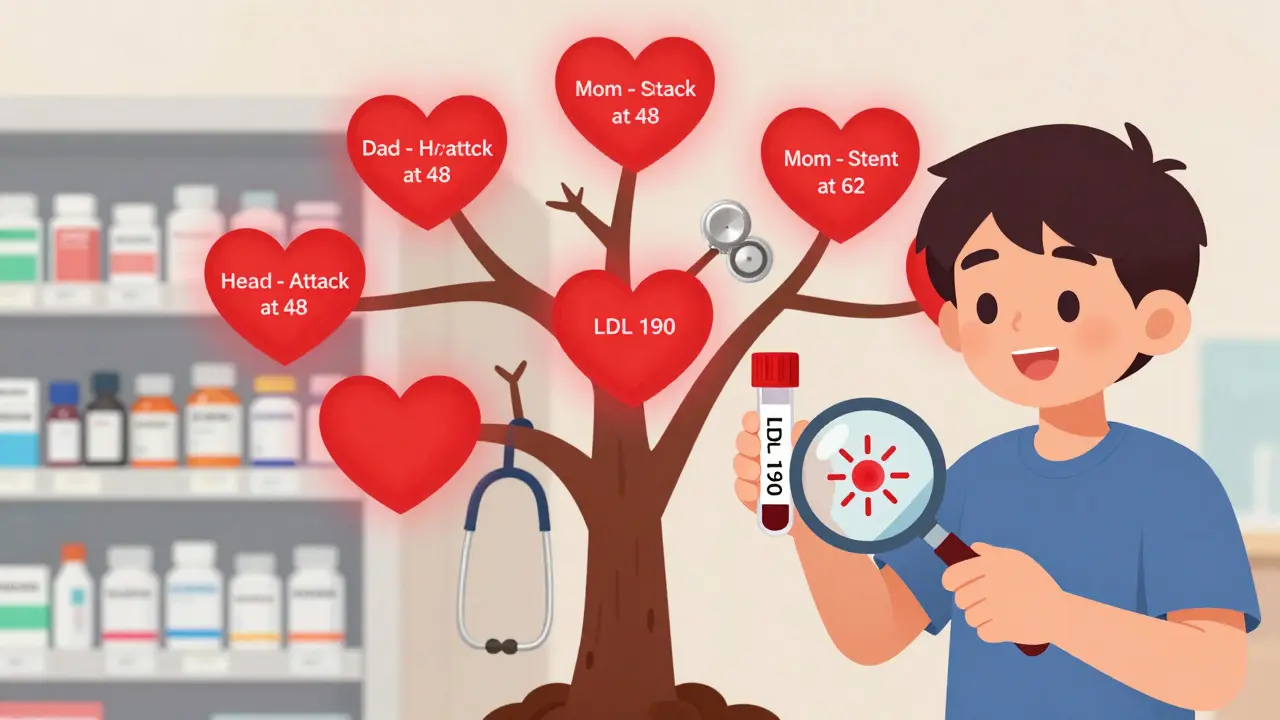
Cholesterol: It’s Not Just About the Number
Cholesterol gets a bad rap, but it’s not the villain. It’s the imbalance. When LDL (the “bad” cholesterol) builds up in your arteries, it forms plaques. The American Heart Association says 94 million U.S. adults have LDL levels too high. That’s 38% of the population. Each 10-point rise in LDL increases heart disease risk by about 5%. But here’s what most people miss: HDL (the “good” cholesterol) matters too. Low HDL is just as dangerous as high LDL. And triglycerides? If they’re over 150, they’re adding fuel to the fire. Statins work - and they’re not scary. High-intensity statins (like atorvastatin 40-80 mg) reduce heart attack risk by 25% to 35% in high-risk people. If your doctor says you need one, listen.Diabetes: The Hidden Heart Disease
Diabetes doesn’t just affect your blood sugar. It wrecks your blood vessels. People with diabetes are two to four times more likely to die of heart disease than those without. And 68% of diabetics over 65 die from cardiovascular problems. Why? High blood sugar damages the lining of your arteries, makes cholesterol stickier, and increases inflammation. Controlling HbA1c below 7% helps - but newer diabetes drugs like SGLT2 inhibitors and GLP-1 agonists do something even better: they directly lower heart risk by 14% to 26%, even beyond glucose control. If you have diabetes, ask your doctor about these options. They’re not just for sugar - they’re for your heart.Weight, Inactivity, and Diet: The Triple Threat
Obesity, lack of movement, and poor diet don’t just add pounds - they add pressure. Together, they raise your risk by 50% or more. Physical inactivity alone causes 6% of global heart disease. Unhealthy diets - high in salt, sugar, and refined carbs - contribute to 11 million deaths worldwide each year. The good news? You don’t need a gym membership. Walking 30 minutes a day, five days a week, cuts heart disease risk by 30%. You don’t need to go keto or vegan. Focus on real food: vegetables, beans, whole grains, nuts, fish. Cut out sugary drinks. Stop eating processed snacks. Small changes, repeated, make a massive difference.How Risk Factors Multiply
The worst scenario isn’t having one risk factor - it’s having three or more. Hypertension plus diabetes? That multiplies your risk by 8 to 10 times. Smoking plus high cholesterol? That’s a perfect storm. The American Heart Association says addressing just three things - smoking, high blood pressure, and physical inactivity - could prevent 45% of heart deaths in the U.S. That’s not a stretch goal. That’s science.What You Can Do Right Now
You don’t need to fix everything at once. Start here:- Get your blood pressure checked - if you haven’t in the last year, do it now.
- Ask for a cholesterol panel - don’t wait for symptoms.
- If you smoke, set a quit date. Use free resources like Quitline or apps like Smokefree.
- Walk for 30 minutes today. No equipment needed.
- Look up your family history. Talk to your parents or siblings. Write it down.
Tools That Help
Doctors use tools like the ASCVD Risk Calculator to estimate your 10-year risk. If you’re over 40, you can use the free version online (from the American College of Cardiology). It asks for your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking history. It gives you a number - low, borderline, intermediate, or high. That number tells you whether you need medication or just lifestyle changes. It’s not perfect, but it’s better than guessing.It’s Not Too Late
A 48-year-old man in a 2022 American Heart Association case study had every risk factor: smoking, high blood pressure, obesity, and a family history of early heart disease. His 10-year risk was 18.2% - almost certain to have a heart attack. After 18 months of quitting smoking, losing weight, taking statins, and walking daily, his risk dropped to 6.3%. He didn’t just avoid a heart attack - he rewrote his future. You can too.Can you have heart disease even if you’re young?
Yes. While heart disease is more common after 45, it can strike younger people - especially if they have strong family history, diabetes, smoking, or inherited conditions like familial hypercholesterolemia. Cases of heart attacks in people under 35 are rising, often linked to lifestyle and genetics.
Is family history the same as genetics?
Family history is a sign that genetics may be playing a role, but it’s not the whole story. Shared lifestyle habits - like poor diet or smoking - also contribute. Still, if close relatives had early heart disease, your genetic risk is higher. Genetic testing for conditions like familial hypercholesterolemia can confirm whether you carry specific high-risk variants.
Does quitting smoking really help if you’ve smoked for decades?
Absolutely. Within one year of quitting, your heart disease risk drops by half. After 15 years, it’s nearly the same as someone who never smoked. Even if you’ve smoked for 30 years, quitting now still adds years to your life. The damage isn’t permanent - your body starts healing the moment you stop.
Can you lower your risk if you have diabetes?
Yes, and more than you might think. Controlling blood sugar helps, but newer diabetes medications like SGLT2 inhibitors and GLP-1 agonists also directly protect your heart. They reduce heart attack risk by 14% to 26% beyond glucose control. Talk to your doctor - these aren’t just for sugar management.
Do I need medication to manage heart disease risk?
Not always. For many people, lifestyle changes alone are enough - especially if your risk is low or borderline. But if your 10-year risk is above 20%, or you have diabetes, high blood pressure, or very high cholesterol, medication like statins or blood pressure pills is proven to save lives. It’s not a failure - it’s smart prevention.








kirti juneja
This post hit me right in the feels. I’m 32, Indian, and my dad had a stent at 47. I thought I was invincible until I saw my LDL was 180. Started walking daily, swapped chai for green tea, and yes-I’m actually eating veggies now. 🌱 No fancy diet, just less junk. My cardiologist said I’m already ahead of 90% of people my age. You don’t need to be perfect, just persistent.