Statin-Antifungal Interaction Risk Checker
Assess Your Risk
Select your statin and antifungal to see the risk level and recommendations.
HIGH RISK
This combination significantly increases risk of severe muscle damage (myopathy) and rhabdomyolysis.
Recommended action:
Immediately switch to a non-interacting statin (pravastatin or rosuvastatin) or consider alternative antifungal. Do not continue this combination.
When you’re taking a statin to lower cholesterol and then get prescribed an azole antifungal for a stubborn fungal infection, you might not think twice about combining them. But this common combo can quietly push your body toward a dangerous tipping point-severe muscle damage, liver stress, and even hospitalization. It’s not rare. It’s not theoretical. It’s happening to thousands of people every year, and most don’t see it coming.
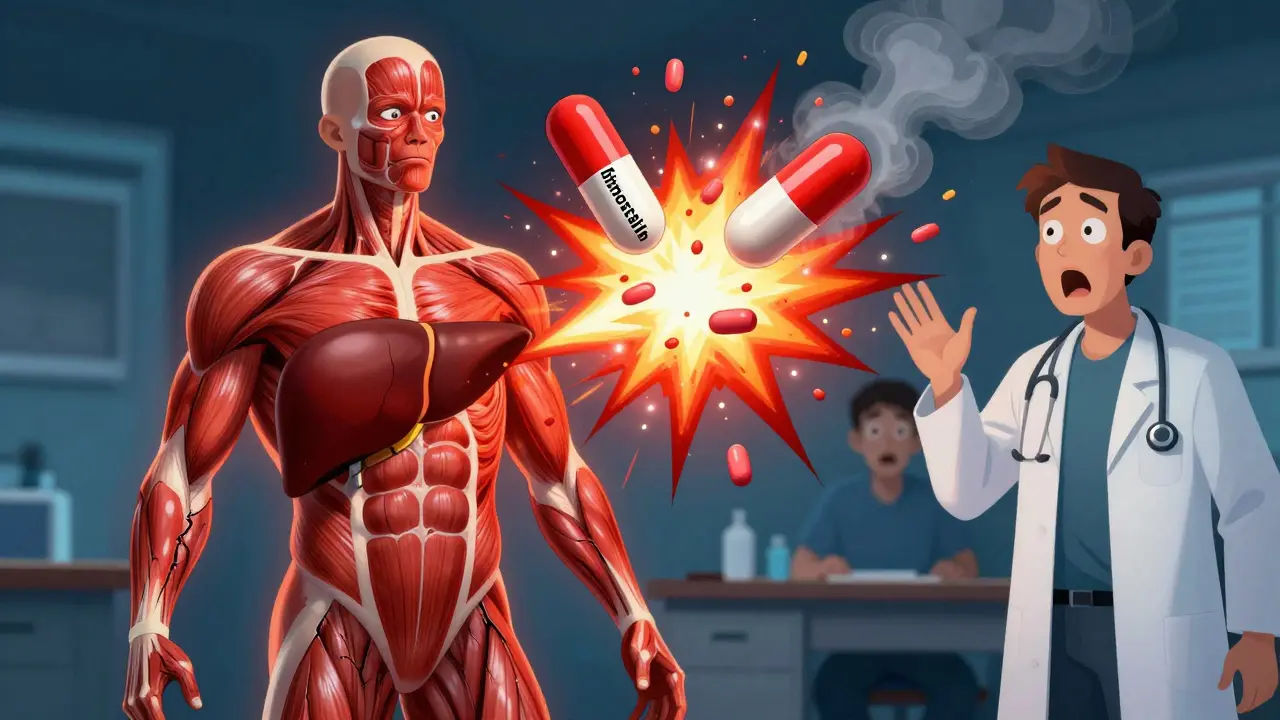
Why This Interaction Is So Dangerous
Statins like simvastatin, lovastatin, and atorvastatin work by blocking an enzyme in your liver that makes cholesterol. But they’re also broken down by a liver enzyme called CYP3A4. Azole antifungals-drugs like itraconazole, ketoconazole, and posaconazole-shut down that same enzyme. When they do, your statin doesn’t get cleared from your body like it should. Instead, it builds up. And when statin levels climb too high, your muscles start to break down.
This isn’t just muscle soreness. This is myopathy-a condition where muscle fibers die, leak proteins into the bloodstream, and can lead to rhabdomyolysis, a life-threatening breakdown of muscle tissue that can crush your kidneys. The baseline risk of myopathy from statins alone is around 0.1%. But when you add a strong CYP3A4 inhibitor like itraconazole? That risk jumps to 1-5%. In some cases, it’s even higher.
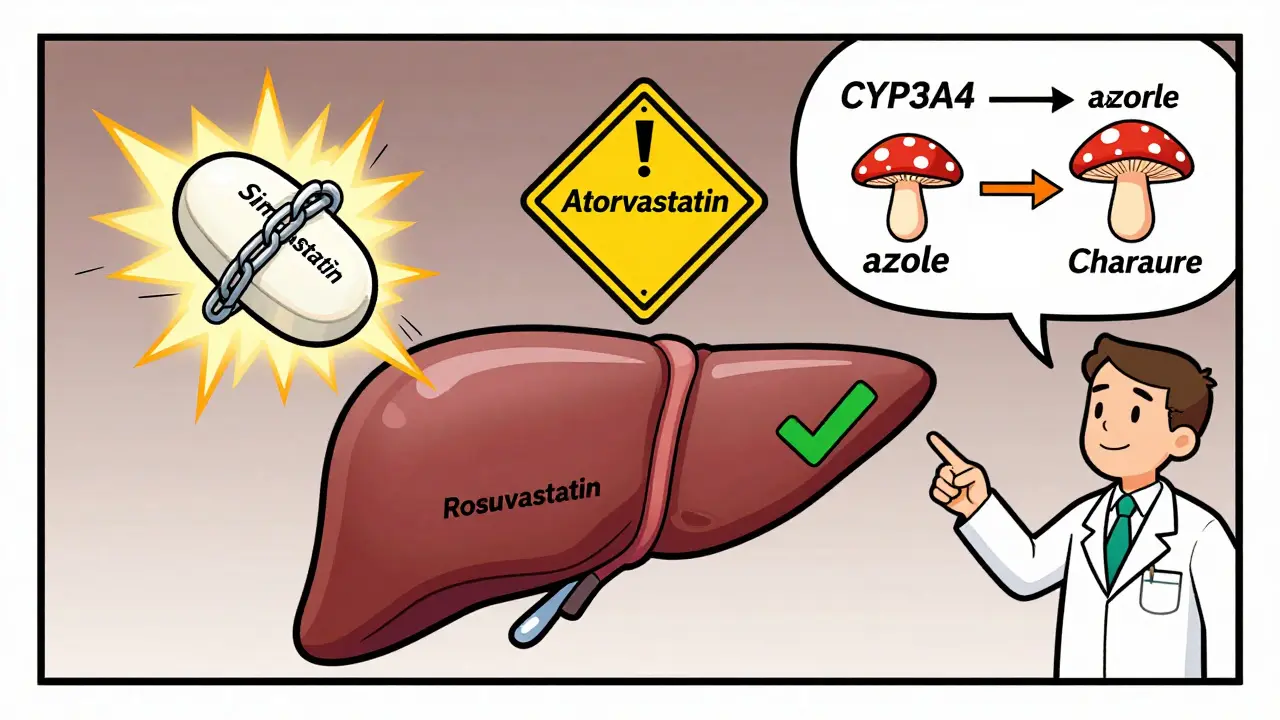
Not All Statins Are Created Equal
Here’s the critical part: not every statin carries the same risk. If you’re on simvastatin or lovastatin, you’re in the danger zone. Studies show that when itraconazole is added, simvastatin levels can spike by more than 10 times. That’s not a typo. Ten-fold. That’s why the FDA says simvastatin over 20 mg should never be taken with strong CYP3A4 inhibitors. Lovastatin has the same warning.
Atorvastatin? It’s risky too, but less so. Its levels can still double or triple with azoles, which is why doctors limit it to 20 mg daily when used together. But here’s the good news: pravastatin and rosuvastatin barely touch CYP3A4. They’re cleared through other pathways. That means when you need an antifungal, switching to one of these two can cut your risk by 80% or more.
What About Other Azoles?
Fluconazole is often seen as the "safer" azole because it mainly blocks CYP2C9, not CYP3A4. But even it can bump up simvastatin levels by nearly 2 times. Voriconazole? Still a moderate inhibitor. Itraconazole and posaconazole? They’re the worst offenders. And isavuconazole? It’s the new kid on the block-and it’s the mildest, with almost no effect on statin levels.
So if you’re on a statin and need an antifungal, the choice matters. If you’re on simvastatin and your doctor prescribes itraconazole for a fungal nail infection? That’s a red flag. If you’re on rosuvastatin and prescribed isavuconazole? That’s manageable.
The Real Cost: Muscle Pain, Hospitalizations, and Lost Trust
Patients don’t always report mild muscle aches. They think it’s just aging, or they’re out of shape. But when muscle pain hits hard-cramps, weakness, dark urine-it’s too late. The FDA’s adverse event database shows over 1,800 reports of myopathy linked to statin-azole combos between 2015 and 2022. Simvastatin with itraconazole alone made up nearly 800 of those cases.
One patient on Reddit described going from hiking every weekend to barely walking after 10 days on fluconazole and 20 mg simvastatin. His CK levels (a marker of muscle damage) hit 18,400 U/L. Normal is under 195. He spent five days in the hospital. That’s not an outlier. That’s a pattern.
Surveys show 24% of statin users quit their medication when an azole antifungal was added. Why? Because the muscle pain was unbearable. And many never went back. That’s a huge problem-uncontrolled cholesterol can lead to heart attacks and strokes. So the trade-off isn’t just about side effects. It’s about survival.
What Doctors Should Do
Good prescribing means knowing the metabolism map. If you’re a clinician and you’re about to prescribe itraconazole to someone on simvastatin, you have three options:
- Switch the statin to pravastatin or rosuvastatin before starting the antifungal.
- Temporarily stop the statin during the antifungal course (if cholesterol control isn’t urgent).
- Use a non-azole antifungal like terbinafine (for nail fungus) or an echinocandin (for systemic infections).
For older adults-especially over 65-the risk doubles. The American Geriatrics Society says to avoid these combinations entirely in that group. Liver function tests should be checked before and after starting the combo. CK levels? Monitor them weekly for the first month. Don’t wait for symptoms.

What Patients Should Do
If you’re on a statin and your doctor says you need an antifungal, ask:
- Which one are you prescribing?
- Is it a strong CYP3A4 inhibitor?
- Can we switch my statin to something safer?
- Should I get my CK or liver enzymes checked before we start?
Don’t assume your pharmacist caught it. Even with automated alerts, 1 in 5 prescriptions still slip through. If you start feeling unexplained muscle pain, weakness, or dark urine, stop the meds and call your doctor immediately. Don’t wait. Don’t ignore it.
The Future: Safer Choices Are Here
There’s new hope. Bempedoic acid (ETC-1002) was approved in 2020. It lowers cholesterol without touching CYP3A4. It doesn’t cause muscle pain. It’s not a statin-but it works. And it’s growing in use. By 2023, over 5% of new cholesterol prescriptions were for this drug. That number will climb.
Genetic testing is also getting smarter. Some people have a gene variant (SLCO1B1) that makes them clear statins slower. If you’re one of them, even normal statin doses can be risky. The FDA now recommends testing for this if you need to combine statins with azoles. It’s not routine yet-but it should be.
Bottom Line
This interaction isn’t a footnote. It’s a major clinical hazard. The data is clear: simvastatin and itraconazole together are a dangerous pair. Lovastatin and posaconazole? Same story. But the fix is simple: switch to pravastatin or rosuvastatin. Use non-azole antifungals when possible. Monitor your body. Speak up.
Statin therapy saves lives. Azole antifungals save lives too. But when they’re paired without care, they can do harm. Knowledge isn’t just power-it’s protection. Ask the questions. Make the switch. Your muscles-and your heart-will thank you.
Can I take fluconazole with my statin?
Fluconazole is a weaker inhibitor than itraconazole or ketoconazole, but it can still raise statin levels-especially simvastatin and lovastatin. If you’re on simvastatin or lovastatin, avoid fluconazole if possible. If you must take it, switch to pravastatin or rosuvastatin first. Monitor for muscle pain. Fluconazole is safer with atorvastatin at 20 mg or less, but still not risk-free.
What are the signs of statin-induced myopathy?
Early signs include unexplained muscle aches, cramps, or weakness, especially in the shoulders, thighs, or lower back. As it worsens, you may feel stiff, tired, or notice dark brown urine (a sign of muscle breakdown). If you have these symptoms after starting an azole antifungal, stop the statin and contact your doctor immediately. A simple blood test for CK (creatine kinase) can confirm muscle damage.
Is it safe to take statins and antifungals if I take them at different times of day?
No. Spacing them out-like taking statins in the morning and azoles at night-doesn’t help. The problem isn’t timing. It’s that the azole shuts down your liver’s ability to break down the statin for days. Even if you take them 12 hours apart, the enzyme is still blocked. The only safe approach is switching to a non-interacting statin or antifungal.
Why do some statins cause more muscle pain than others?
It comes down to how they’re processed and their chemical form. Simvastatin and lovastatin are fat-soluble lactones that easily enter muscle cells. Once inside, they disrupt mitochondrial function and protein production. Pravastatin and rosuvastatin are water-soluble and don’t penetrate muscle tissue as deeply. They’re also cleared by different liver enzymes, so they’re less affected by azoles. That’s why they’re the preferred choices.
What if I can’t switch my statin because my cholesterol is high?
If you’re on a high-risk statin and need long-term antifungal therapy, talk to your doctor about alternatives. Bempedoic acid (ETC-1002) is a non-statin option that doesn’t interact with azoles. Ezetimibe, PCSK9 inhibitors, or dietary changes can also help. Don’t accept muscle pain as unavoidable. There are other ways to control cholesterol without risking your muscles.