Hepatic Encephalopathy: Causes, Signs, and How Medications Affect It
When your liver can’t clean your blood properly, toxins like ammonia, a waste product from protein breakdown that builds up when the liver fails flood your brain. This is hepatic encephalopathy, a reversible brain disorder caused by severe liver damage. It doesn’t mean you’re losing your mind—it means your liver is failing to do its job, and your brain is paying the price. Also known as liver brain syndrome, it shows up as confusion, forgetfulness, slurred speech, or even coma in advanced cases.
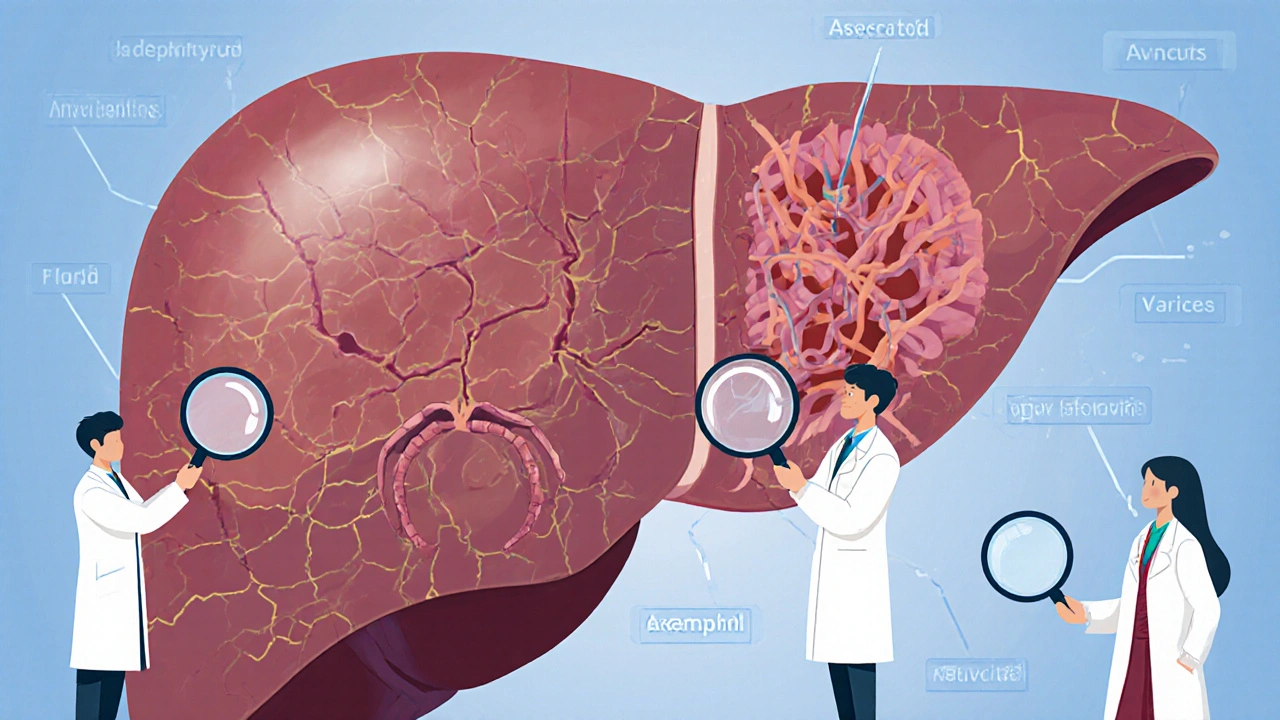
Most people with hepatic encephalopathy, a complication of cirrhosis or acute liver failure have underlying liver disease, often from years of alcohol use, hepatitis, or fatty liver. But it’s not just the liver that’s at fault. A portosystemic shunt, an abnormal pathway that lets blood bypass the liver—whether natural or surgically created—can let toxins slip straight into your bloodstream. And here’s the catch: some common meds make it worse. Antibiotics like rifaximin help, but sedatives, painkillers, and even antacids can push you over the edge. That’s why people with liver problems need to be extra careful with what they take.
It’s not just about avoiding bad drugs—it’s about timing, diet, and monitoring. High protein meals can spike ammonia levels, but cutting protein too much makes muscle loss worse. It’s a tightrope walk. That’s why doctors often recommend lactulose or rifaximin to trap toxins in the gut before they reach the brain. And if you’re noticing changes in your thinking, mood, or coordination, don’t brush it off as "just getting older." It could be your liver screaming for help.
What you’ll find below are real stories and science-backed guides on how medications, diet, and monitoring tools affect hepatic encephalopathy. From how anticholinergic drugs mimic dementia symptoms in seniors to how protein timing can make or break your treatment, these posts give you the practical tools to protect your brain when your liver is struggling.
Cirrhosis is the advanced stage of chronic liver disease, marked by scarring and declining function. Learn about its major complications-ascites, bleeding, brain fog, and cancer-and how to manage them with diet, meds, and monitoring.