Insurance Formulary: What It Is and How It Affects Your Medication Costs
When you fill a prescription, what you pay isn’t just about the drug—it’s about your insurance formulary, a list of medications approved and covered by your health plan, organized by cost tiers and restrictions. Also known as a drug list, it’s the hidden rulebook that decides if your medicine is in, out, or requires paperwork before you can get it. Most people don’t realize their plan doesn’t cover everything—even if it’s FDA-approved. Your formulary controls what you pay out of pocket, whether you need prior authorization, and sometimes even if you can get the drug at all.
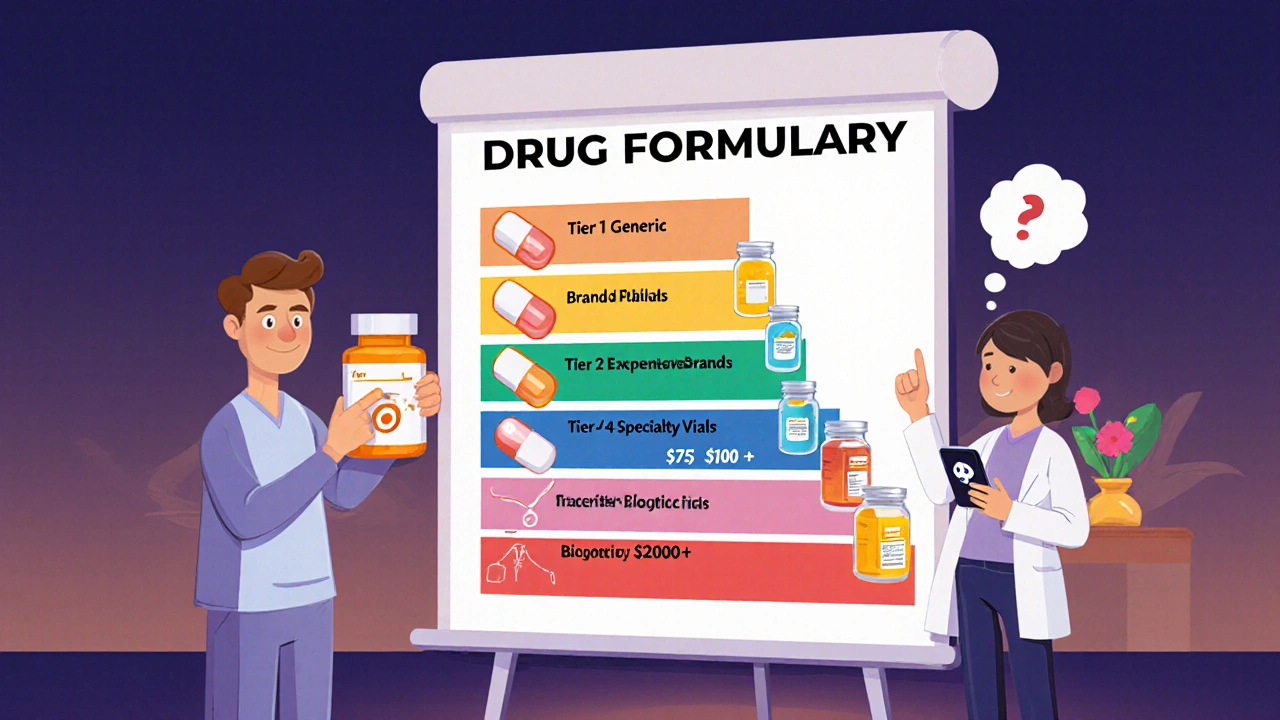
Formularies are split into tiers, categories that determine your cost-sharing, from lowest to highest. Tier 1 usually includes generic drugs like metformin or levothyroxine, costing just a few dollars. Tier 2 might be brand-name drugs with generic alternatives. Tier 3 and 4? Those are specialty meds like SGLT-2 inhibitors or biologics for autoimmune diseases—and they can cost hundreds. Some plans even have a Tier 5 for ultra-expensive drugs, like those used for rare conditions. If your drug is on a higher tier, you’re paying more, plain and simple. That’s why prior authorization, a process where your doctor must prove to the insurer that a drug is medically necessary before coverage is granted. Also known as pre-approval, it’s common for drugs like azithromycin for empyema or voriconazole for Candida infections, especially when cheaper options exist. You might get a call from your pharmacy saying your prescription is on hold—not because they ran out, but because your insurer needs more info.
And it’s not just about cost. Formularies change often. A drug you’ve taken for years can suddenly be moved to a higher tier—or dropped entirely—without warning. That’s why people on long-term meds for diabetes, liver disease, or thyroid conditions need to check their formulary every year during open enrollment. If your plan drops your drug, you might need to switch to an alternative like ibuprofen instead of diclofenac, or try a different diabetes combo like Actoplus Met instead of Foracort Inhaler. Your pharmacist can help you find a covered substitute, but you have to ask.
Some drugs are restricted because of safety risks. Fournier’s gangrene linked to SGLT-2 inhibitors? That’s why insurers now require stricter monitoring before approving those meds. Or take terbutaline during pregnancy—many plans limit it because of fetal risks. Even something as common as antihistamines can be flagged if they interact with blood pressure meds. These aren’t random rules. They’re based on real data, like medication error statistics or QT prolongation risks from macrolides. Insurers use that data to control costs and reduce harm.
But here’s the thing: just because a drug isn’t on your formulary doesn’t mean you can’t get it. You can appeal. Your doctor can file a form explaining why a non-formulary drug is essential. Many appeals succeed, especially when there’s evidence—like how dimethyl fumarate shows promise for fibromyalgia, even if it’s not yet a standard choice. You can also ask for a temporary exception while you wait for approval. And if you’re buying generic Topamax online, make sure the pharmacy is in-network. Out-of-network purchases won’t count toward your formulary coverage.
Knowing your formulary isn’t just about saving money—it’s about avoiding treatment gaps. If your insulin runs out during a shortage, your formulary might list alternatives. If you’re on levothyroxine and take calcium, your formulary might require you to space them out. It’s the roadmap to getting the right drug at the right price. Below, you’ll find real-world guides on how to navigate these systems, spot hidden restrictions, and fight for the meds you need—without letting bureaucracy stand in your way.
A drug formulary is your insurance plan's list of covered medications. Learn how tiers, exceptions, and new 2025 rules affect your out-of-pocket costs and how to find the best coverage for your prescriptions.