Anaphylaxis Recognition Tool
Check Your Symptoms
Answer the following questions based on symptoms occurring within 30 minutes of medication exposure (or up to 6 hours for oral drugs).
Results will appear here after checking symptoms...
When a medication triggers a severe allergic reaction, it doesn’t just cause a rash or sneezing-it can shut down your body in minutes. Anaphylaxis from drugs is not rare. It happens in hospitals, clinics, and even at home after a prescription is filled. And too often, it’s missed until it’s almost too late.
What Anaphylaxis Really Looks Like
Anaphylaxis isn’t just "a bad allergy." It’s a full-body emergency. Your immune system overreacts to a medication, releasing chemicals that cause your blood vessels to leak, your airways to tighten, and your blood pressure to crash. Symptoms can start in under five minutes after an IV drug, or up to six hours after taking a pill.The signs are often confusing. One person might break out in hives. Another might feel dizzy, then can’t breathe. A third might vomit and go pale. There’s no single pattern. That’s why so many get misdiagnosed as panic attacks, heart problems, or even side effects of the drug itself.
According to the American Academy of Allergy, Asthma & Immunology, you’re likely having anaphylaxis if:
- You have skin symptoms (hives, swelling, flushing) and trouble breathing or low blood pressure
- Two or more body systems are involved-skin, lungs, heart, gut-after taking a medication
- Your blood pressure drops sharply after exposure to a known drug trigger
These aren’t guesses. They’re the 2023 clinical guidelines backed by data from over 12,000 cases. And the numbers don’t lie: medication-induced anaphylaxis causes 15% of all cases, and it’s deadlier than food-triggered reactions.
Which Medications Are Most Likely to Trigger It?
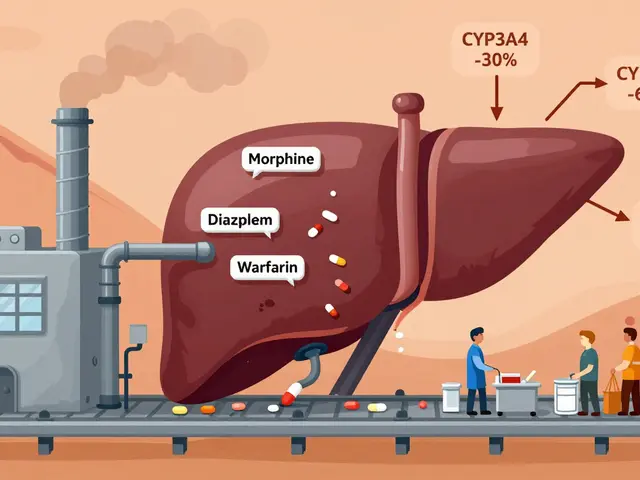
Not all drugs carry the same risk. Some are far more dangerous than others.Antibiotics are the #1 culprit. Penicillin and related drugs like amoxicillin account for 70-80% of all antibiotic reactions. That’s why doctors ask about penicillin allergies before prescribing anything. But here’s the catch: many people think they’re allergic because they had a rash as a kid-but 90% of them aren’t truly allergic anymore. Still, if you’ve had a real reaction before, you’re at high risk.
Other common triggers:
- NSAIDs like ibuprofen and naproxen (15% of cases)
- Monoclonal antibodies like rituximab and cetuximab (used in cancer and autoimmune diseases)
- Chemotherapy drugs, especially platinum-based ones
- IV contrast dye used in CT scans
Even something as common as vancomycin-an antibiotic given in hospitals-can cause a reaction that looks like anaphylaxis. But it’s not always true anaphylaxis. Sometimes it’s "red man syndrome," a histamine release that causes flushing and itching but no drop in blood pressure or breathing trouble. Mistaking one for the other can delay life-saving treatment.
Why It’s So Deadly in Medical Settings
You’d think hospitals are safe places for reactions. But they’re not. In fact, medication-induced anaphylaxis is more likely to kill you in a hospital than at home.Why? Because symptoms are often blamed on something else. Low blood pressure? Must be the anesthesia. Trouble breathing? Must be fluid overload. Skin rash? Must be a virus. A 2022 JAMA study found that 41.7% of drug-induced anaphylaxis cases are initially misdiagnosed. And when that happens, epinephrine-the one drug that can save your life-isn’t given.
Here’s the brutal truth: if epinephrine isn’t given within 30 minutes of symptom onset, your chance of dying triples. In 78% of fatal cases, epinephrine was either delayed or never given. That’s not because doctors are careless. It’s because the signs are subtle, and the pressure is high.
One ER doctor in Massachusetts described a case where a 68-year-old patient got IV contrast, went pale, and dropped blood pressure. The team thought it was a vasovagal reaction-common during scans. It wasn’t until the patient started wheezing and her oxygen levels crashed to 82% that someone shouted, "It’s anaphylaxis!" Epinephrine was given. She recovered. But she almost didn’t make it.
What to Do-Right Now
If you or someone else shows signs of anaphylaxis after taking a medication, there’s only one rule: act fast.Step 1: Use epinephrine immediately. Inject it into the outer thigh, even through clothing. Adults need 0.3-0.5 mg. Don’t wait. Don’t call 911 first. Don’t give antihistamines. Epinephrine is the only thing that stops the reaction from killing you.
Step 2: Call emergency services. Even if you feel better after epinephrine, you still need to go to the hospital. Symptoms can come back-sometimes hours later.
Step 3: Stay lying down. Sitting up or standing can cause your blood pressure to drop further. Lie flat with legs elevated if possible.
Step 4: Don’t rely on inhalers or antihistamines alone. They help with symptoms, but they won’t stop the body from shutting down. Epinephrine is the only treatment that works.
The American Heart Association says 87% of people who survive anaphylaxis got epinephrine correctly and quickly. That’s not luck. It’s action.
What Happens After
Surviving anaphylaxis doesn’t mean you’re done. You need follow-up care.First, you need an epinephrine auto-injector-two of them-and you need to know how to use them. Yet, over half of patients who survive a drug-induced reaction never get one prescribed. That’s a massive gap in care.
Second, you need allergy testing. A skin test or blood test can confirm what triggered the reaction. This isn’t just for peace of mind. It’s to prevent the next one. If you’re allergic to penicillin, you’ll be given safer alternatives. If you’re allergic to a chemotherapy drug, desensitization protocols can sometimes let you safely receive it again.
Third, your medical records must be updated. The European Academy of Allergy found that 63% of medication errors leading to anaphylaxis happened because the allergy wasn’t properly recorded in electronic health records. That’s on the system. But you can help: carry a medical alert card or wear a bracelet. Tell every doctor, nurse, and pharmacist you see.

What’s Changing in 2026
The tide is turning. New tools are emerging to stop anaphylaxis before it starts.In 2023, the FDA approved the first rapid blood test for penicillin allergy-results in 15 minutes. It’s accurate 93% of the time. No more guessing. No more avoiding penicillin for life if you’re not truly allergic.
Hospitals are using AI to predict who’s at risk. The NIH’s Anaphylaxis Prediction Algorithm looks at your EHR-past reactions, family history, current meds-and flags high-risk patients before they get a new drug. Early results show it catches 89% of potential cases.
And by January 1, 2024, every accredited U.S. hospital must have an anaphylaxis response protocol. That means staff are trained. Epinephrine is stocked in every code cart. Simulation drills are mandatory. The goal? Cut deaths by 50% by 2030.
But technology won’t fix everything. In low-resource settings, people still die because epinephrine isn’t available. Training still lags. Documentation still fails. The real solution isn’t just better tools-it’s better awareness.
You Can Save a Life
Anaphylaxis from medications is preventable. But only if you know what to look for.If you’ve ever had a reaction to a drug-even if it was "just a rash"-don’t ignore it. Get tested. Document it. Carry epinephrine if you’re at risk.
If you’re a caregiver, a nurse, or a family member-learn the signs. Know how to use an auto-injector. Don’t wait for someone else to act.
Anaphylaxis doesn’t give you time to think. But you can give yourself the edge-by knowing, by preparing, by acting fast.
One injection. One minute. One life.









Gaurav Meena
Just had my kid go into anaphylaxis after amoxicillin last year. We thought it was a rash until she couldn’t breathe. Epinephrine saved her. I carry two auto-injectors now. Don’t wait. Don’t hope. Act. 🙏
Jodi Olson
It’s astonishing how medicine still treats anaphylaxis as an edge case rather than a systemic failure. The data is clear. The protocols exist. Yet we rely on individual heroism instead of institutional accountability. Epinephrine should be as ubiquitous as fire extinguishers.
calanha nevin
As a nurse in a rural ER, I’ve seen this too many times. A patient gets contrast, goes pale, and the team says it’s vasovagal. Ten minutes later, they’re coding. We now have a checklist posted above every contrast cart. Epinephrine is the first thing we grab-not after, not if, but immediately. Training saved three lives last quarter. This isn’t theory. It’s practice.
Sidhanth SY
My uncle died from this in 2019. They thought it was a heart attack. He had a rash and was dizzy. No one connected the dots. I still get angry thinking about it. But now I carry epinephrine everywhere. Even to the gym. People think I’m overreacting. I’m just not willing to gamble with my life anymore.
Adarsh Uttral
penicillin allergies are so overdiagnosed like 90% of ppl think they have it but dont. i got tested last year turns out i was fine. now i can take amoxicillin again. saved me like 3k in meds. get tested ppl its easy
Niamh Trihy
That JAMA study about 41.7% misdiagnosis rate? That’s the tip of the iceberg. I work in ICU. We’ve had cases where patients were given beta-blockers after anaphylaxis because they thought it was arrhythmia. Beta-blockers can kill you in this scenario. We need mandatory anaphylaxis modules for all med students. Not optional. Required.
Diana Dougan
Oh wow anaphylaxis? How quaint. Next you’ll tell me water is wet. I’m sure the 12,000 cases you cited are all perfectly documented and not just people who got hives and panicked. Also, epinephrine? Isn’t that just adrenaline? Why not just drink coffee?
Bobbi Van Riet
I’ve been on so many meds that caused reactions-ibuprofen gave me hives once, vancomycin made me flush like I’d run a marathon in a sauna-but I never thought it was anaphylaxis until my mom had a full-blown episode after a CT scan. I didn’t know the difference between red man syndrome and real anaphylaxis until I watched her turn blue. Now I have a laminated card in my wallet with the symptoms and the emergency steps. I even taught my 14-year-old how to use the injector. It’s not fear. It’s responsibility.
Holly Robin
THEY’RE HIDING THE TRUTH. EPINEPHRINE ISN’T THE ANSWER-IT’S THE DISTRACTION. WHY AREN’T THEY TESTING PHARMACEUTICAL COMPANIES FOR INTENTIONAL REACTION INDUCTION? THE FDA IS IN BED WITH BIG PHARMA. YOU THINK THEY WANT YOU TO KNOW HOW MANY DRUGS ARE DESIGNED TO KILL? THEY’RE PROFITING FROM THE PANIC. I’VE SEEN THE DOCUMENTS. THEY KNOW. THEY JUST DON’T CARE. #ANAPHYLAXISCONSPIRACY
Shubham Dixit
In India, we don’t have epinephrine in every clinic. We don’t even have proper EHRs. And you’re talking about AI algorithms and FDA protocols? That’s a luxury. We lose people every day because the nearest hospital is 50km away and the ambulance doesn’t have adrenaline. This article reads like it was written for Beverly Hills. We need basic access first-not fancy tech. Stop preaching to the privileged.
KATHRYN JOHNSON
Epinephrine is not a cure. It’s a bandage on a ruptured artery. The real failure is systemic: inadequate training, fragmented records, and the illusion of safety in institutional settings. Until we treat anaphylaxis as a systems engineering problem-not a medical emergency-we will keep burying people who were never given a chance.