Premenstrual Dysphoric Disorder is a severe mood disorder that occurs in the luteal phase of the menstrual cycle, characterized by intense emotional, physical, and behavioral symptoms that interfere with daily life. It affects roughly 3‑5% of menstruating individuals and is distinct from typical premenstrual syndrome because the symptoms are disabling and often require clinical intervention.
Quick Takeaways
- PMDD involves hormone‑driven mood changes that peak 1‑2 weeks before menstruation.
- Psychoeducation equips individuals with a clear framework of what’s happening in the body and brain.
- Knowing the symptom pattern reduces anxiety and improves treatment adherence.
- Practical tools include symptom diaries, CBT techniques, and peer support.
- Early psychoeducation can prevent crisis situations and empower self‑advocacy.
What Exactly Is PMDD?
PMDD belongs to the broader category of menstrual‑related mood disorders. The condition follows a predictable timeline: symptoms start during the follicular phase, crescendo in the luteal phase, and resolve with the onset of menses. Common complaints include severe irritability, anxiety, depression, fatigue, and physical aches.
Research links the disorder to rapid shifts in estrogen and progesterone, which in turn affect neurotransmitters such as serotonin. For many, the brain’s response to these hormonal swings is exaggerated, resulting in the emotional turbulence that defines PMDD.
Defining Psychoeducation
Psychoeducation is a systematic approach that combines information, coping strategies, and skill‑building to help people understand a health condition. Rather than merely delivering facts, it translates complex medical language into relatable examples, empowering patients to make informed decisions.
In the context of PMDD, psychoeducation does three things:
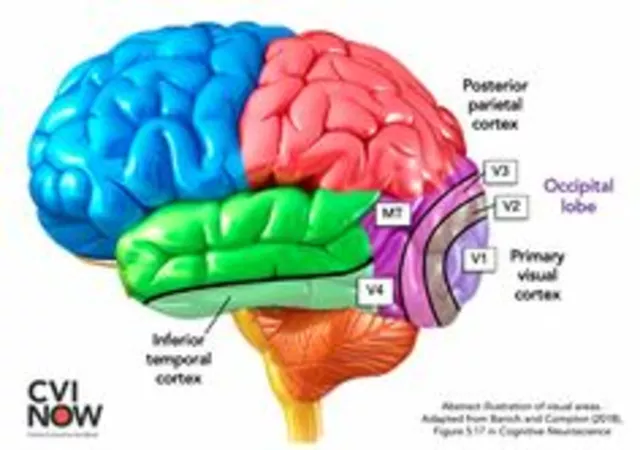
- Explains the hormonal and neurochemical mechanisms behind the symptoms.
- Normalizes the experience, reducing shame and self‑blame.
- Provides a toolbox of behavioral and therapeutic options.
Why Psychoeducation Matters for PMDD
Many people with PMDD spend months or years attributing their mood swings to personal weakness, relationship problems, or work stress. When the underlying physiological driver finally surfaces, relief is often immediate. This shift from self‑diagnosis to medical understanding is the core benefit of psychoeducation.
Key impacts include:
- Reduced anxiety: Knowing that symptoms will subside with the menstrual flow removes the fear of an “unknown” crisis.
- Improved treatment adherence: Patients who understand why an SSRI is prescribed during the luteal phase are more likely to take it consistently.
- Better communication: Armed with the right vocabulary, individuals can explain their condition to partners, employers, and clinicians without stigma.
Core Components of an Effective Psychoeducational Program
A well‑rounded program blends several elements:
- Symptom Diary: Tracking mood, physical sensations, and cycle dates for at least two cycles creates a pattern that validates the diagnosis.
- Educational Handouts: Simple graphics that show hormone curves, brain‑neurotransmitter links, and common triggers.
- Cognitive Behavioral Therapy (CBT) Techniques: Identifying negative thought loops that intensify symptoms and replacing them with balanced perspectives.
- Peer Support Groups: Sharing experiences normalizes feelings and introduces practical coping tips.
- Professional Guidance: Coordination with gynecologists or mental‑health providers to tailor medication or therapy.

Step‑by‑Step Guide to Start Your Psychoeducation Journey
- Confirm the Diagnosis: Schedule an appointment with a health professional experienced in PMDD. Bring a month‑long symptom diary to support the discussion.
- Gather Reliable Resources: Look for materials from reputable organizations such as the American College of Obstetricians and Gynecologists (ACOG) or the International Society for Premenstrual Disorders.
- Start a Digital or Paper Diary: Record daily mood scores (0‑10), specific physical symptoms, and the start/end dates of your period. Apps like Clue or Flo have built‑in tracking modes.
- Learn the Hormone‑Brain Connection: Review how estrogen and progesterone fluctuations influence serotonin pathways. Understanding this link demystifies why mood changes feel out of control.
- Practice CBT Skills: Identify a recurring negative thought (e.g., “I’m a terrible partner when I’m irritable”). Challenge it with evidence (“I’m irritable only 4‑5 days a month and still love my partner”). Write the balanced statement in your diary.
- Join a Support Community: Online forums, local meet‑ups, or therapist‑led groups provide peer validation and practical tips (like timing exercise or nutrition adjustments).
- Review Treatment Options: Discuss lifestyle changes, SSRIs, hormonal contraceptives, or emerging treatments like luteal‑phase GnRH antagonists with your provider. Psychoeducation helps weigh benefits versus side‑effects.
- Re‑evaluate Every 3‑6 Months: Use your diary data to assess whether symptoms have improved, remained stable, or worsened. Adjust the plan accordingly.
Common Pitfalls and How to Avoid Them
Even with the best intentions, people can stumble:
- Information Overload: Too many scientific articles can be overwhelming. Stick to a handful of vetted sources.
- Self‑Medication: Using over‑the‑counter supplements without professional guidance may interfere with prescribed drugs.
- Ignoring Comorbidities: Anxiety or depression often co‑occur with PMDD. Treat each condition openly rather than assuming they’re the same.
- Inconsistent Diary Entry: Skipping days creates gaps that reduce the diary’s diagnostic power.
- Social Isolation: Feeling embarrassed can lead to hiding the problem. Regularly engage with trusted friends or support groups.
Address each issue early, and the psychoeducational process stays on track.
Measuring Success: What to Look For
Success isn’t just “feeling better” - it’s measurable changes in several areas:
- Symptom Severity Scores: A drop of at least 30% in diary‑recorded mood scores indicates meaningful progress.
- Functional Improvement: Ability to maintain work performance, relationships, and daily routines during the luteal phase.
- Self‑Efficacy: Confidence in explaining the condition to others and managing triggers without panic.
- Adherence Rates: Consistent medication intake or therapy attendance, often boosted by understanding the why.
Future Directions in PMDD Psychoeducation
Technology is reshaping how we learn about our bodies. Interactive webinars, AI‑driven chatbots, and personalized video modules are emerging to deliver tailored psychoeducation. Researchers are also testing mobile‑based CBT apps that sync with menstrual trackers, providing real‑time coping prompts exactly when hormone levels shift.
Staying informed about these innovations ensures you can adopt the most effective tools as they become available.
Frequently Asked Questions
How is PMDD diagnosed?
A clinician looks for at least five symptoms that appear cyclically, with at least one emotional symptom, and that cause functional impairment. Confirmation requires prospective tracking over two menstrual cycles.
Can lifestyle changes replace medication?
Lifestyle tweaks-regular exercise, balanced diet, adequate sleep-can lessen severity but rarely eliminate moderate‑to‑severe PMDD. Most guidelines recommend combining lifestyle with medication or therapy for optimal results.
What role does CBT play in managing PMDD?
CBT targets the negative thought patterns that amplify emotional symptoms. Structured sessions teach coping skills, stress‑reduction techniques, and cognitive reframing, leading to lower mood‑score ratings during the luteal phase.
Are hormonal contraceptives effective for PMDD?
Combined oral contraceptives that suppress ovulation can stabilize hormone levels and reduce symptoms for many. The specific formulation matters; a provider can help select the most suitable option.
How can I talk to my partner about PMDD?
Use the education handouts as a shared reference, explain the cyclic nature, and express specific needs (e.g., more space during peak days). Emphasizing that the condition is medical, not personal, helps maintain empathy.









Nicole Koshen
Keeping a symptom diary is more than a habit; it’s a data‑driven way to prove to yourself and your clinician that the pattern is real. By rating mood on a 0‑10 scale each day you create a visual curve that mirrors the hormonal swing. When you spot a consistent dip two weeks before menses, you have concrete evidence to discuss treatment options. This also helps you spot triggers-like caffeine or lack of sleep-that may amplify the luteal phase. Over a couple of cycles the diary becomes a powerful advocacy tool, turning subjective feelings into objective numbers.
Ed Norton
Totally agree tracking really helps
Karen Misakyan
The extant literature on Premenstrual Dysphoric Disorder unequivocally establishes its nosological distinction from normative premenstrual syndrome. Empirical investigations have demonstrated that the severity of affective dysregulation correlates with the magnitude of luteal‑phase estrogen and progesterone fluctuations. Consequently, psychoeducational interventions that elucidate these endocrinological mechanisms serve to demystify the phenomenology of the disorder. By presenting a schematic of hormone trajectories alongside neurotransmitter modulation, clinicians facilitate an epistemic shift from self‑blame to informed self‑management. This cognitive reframing is not merely an abstract construct; it bears measurable ramifications for treatment adherence. Studies indicate that patients who comprehend the pharmacodynamic rationale for luteal‑phase selective serotonin reuptake inhibitor administration exhibit higher compliance rates. Moreover, the didactic component empowers patients to articulate their condition with precision in interpersonal contexts, thereby attenuating stigma. The pedagogical framework encompasses symptom quantification, neurobiological exposition, and behavioral skill acquisition. Rigorous diary keeping, for instance, operationalizes the abstract temporal pattern into a quantifiable dataset amenable to statistical analysis. Parallel to this, cognitive behavioral techniques target maladaptive cognitions that exacerbate affective volatility. In sum, the synergistic integration of knowledge transfer and skill development constitutes the essence of psychoeducation. It is incumbent upon practitioners to tailor educational materials to the literacy level and cultural background of each individual. Failure to do so risks engendering a paternalistic dynamic that undermines patient autonomy. Accordingly, the optimal psychoeducational protocol is iterative, incorporating feedback loops that refine content relevance. Ultimately, a well‑instructed patient is better equipped to navigate the cyclic vicissitudes of PMPMDD, thereby enhancing functional outcomes and quality of life.
Amy Robbins
Oh joy, yet another reminder that our brains are basically hormonal roller‑coasters, so let’s all applaud the pharmaceutical industry for turning mood swings into a lucrative market.
Shriniwas Kumar
From a sociocultural epidemiology perspective, the stigmatization of PMDD within collectivist paradigms necessitates a transcultural psychoeducational schema that incorporates both biomedical ontologies and indigenous epistemes, thereby facilitating nosological harmonization across diversified health belief models.
Jennifer Haupt
It is critical to anchor your diary entries within a structured template, noting not only mood intensity but also contextual variables such as sleep hygiene, dietary macronutrient ratios, and psychosocial stressors; this systematic approach yields a multidimensional dataset that clinicians can dissect to calibrate therapeutic regimens with granular precision.
NANDKUMAR Kamble
One cannot overlook the possibility that certain pharmaceutical conglomerates may be capitalizing on the burgeoning awareness of PMDD to market off‑label hormone modulators, a maneuver that aligns neatly with broader narratives of medical commodification hidden beneath a veneer of scientific legitimacy.
namrata srivastava
The epistemic asymmetry inherent in patient‑provider dialogues often perpetuates a hierarchical dissemination of knowledge, wherein the layperson is relegated to a passive receptacle of didactic content rather than an active interlocutor in the co‑construction of therapeutic narratives.
Priyanka arya
Honestly, the whole “just track your mood” vibe feels like a 🎭 mask over a massive pharma plot 😒💊-but hey, if it helps you feel in control, go for it! 🌟🙌
Loren Kleinman
When I first stumbled upon a PMDD pamphlet, I was skeptical about the promise of psychoeducation, assuming it was just another buzzword in the wellness industry. However, after diligently logging my symptoms for three consecutive cycles, patterns emerged that were impossible to ignore. I realized that the intensity of my irritability corresponded almost perfectly with the peaks of luteal‑phase progesterone, a nuance I had never considered. This empirical revelation prompted me to discuss dosage timing with my psychiatrist, who adjusted my SSRI schedule to align with the hormonal surge. The result was a noticeable attenuation of depressive lows during the critical window. Moreover, sharing my diary with a supportive online community yielded practical tips, such as timing moderate exercise after ovulation to harness endorphin release. I also experimented with magnesium supplementation, which seemed to smooth out muscle cramps without interfering with my medication. Over time, the integration of educational resources, self‑monitoring, and collaborative care transformed what once felt like an uncontrollable curse into a manageable rhythm. In hindsight, the psychoeducational framework acted as both a compass and a catalyst, guiding me toward evidence‑based interventions and empowering me to reclaim agency over my own physiological narrative.
Sabrina Goethals
Wow!!! i cant even... ths is so helpful,,, like really, thx for the info!!!
Sudha Srinivasan
Ignoring the science is simply irresponsible; we must all demand accurate information.
Jenny Spurllock
Understanding the neuroendocrine underpinnings of PMDD reshapes how we view emotional resilience and underscores the necessity of integrating mental health education into routine gynecologic care.
Bart Cheever
Looks good but could use less fluff.
Maude Rosièere Laqueille
For anyone starting out, I recommend the ACOG patient guide paired with a simple spreadsheet template; it streamlines data entry and makes trends instantly visible, which can be a game‑changer when discussing options with your provider.