Every time you pick up a prescription, you get a little white or yellow label stuck to the bottle. It looks simple - name, drug, dose, date. But that tiny strip of paper holds everything you need to take your medicine safely. If you don’t understand what it says, you’re not just confused - you’re at risk. Around 1.5 million medication errors happen in the U.S. every year, and many of them start with a label that didn’t make sense.
Your Name Is on There for a Reason
The first thing you see is your name. It’s not just for show. Pharmacists check this every single time they fill a prescription. This is the first line of defense against mixing up medications. You might think, ‘I’m the only one who comes here,’ but pharmacies handle hundreds of prescriptions daily. One wrong name, one misread label, and someone could get the wrong drug. That’s why your name must match exactly what’s on your insurance card or medical record. If it doesn’t, ask the pharmacist to double-check. It’s your right - and your safety.
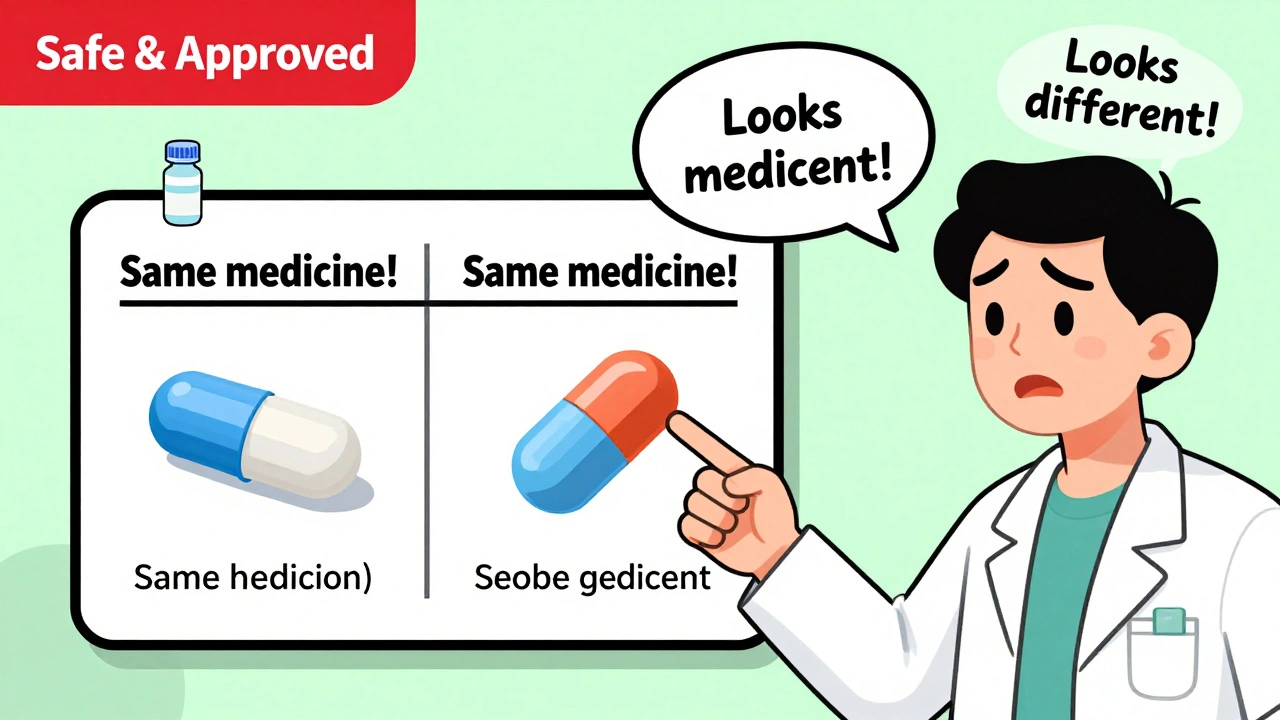
Brand Name vs. Generic Name - What’s the Difference?
You’ll see two names on the label. One is the brand name - like Abstral - and the other is the generic name - fentanyl. The brand name is what the drug company calls it. The generic name is the actual medicine inside. They’re the same thing. Many people panic when they get a different-looking pill and think they were given the wrong drug. But if the generic name matches what your doctor prescribed, you’re fine. Generic drugs are cheaper, just as safe, and approved by the FDA. The only difference is the shape, color, or filler ingredients - nothing that affects how the medicine works.
Dosage: How Much and How Often
This part tells you exactly how much to take and when. It might say: ‘Take one tablet by mouth every 6 hours as needed for pain.’ That means one pill, by mouth, every six hours - not four, not eight. Don’t guess. Don’t assume ‘as needed’ means ‘whenever I feel like it.’ If it says ‘take with food,’ take it with food. If it says ‘take on an empty stomach,’ don’t eat for an hour before or after. The strength is also listed - like ‘100 mcg’ or ‘5 mg.’ That’s the amount of active ingredient. A 5 mg tablet is not the same as a 10 mg tablet. Confusing them can be dangerous. Always check the number. If it looks wrong, ask.
Expiration Date - It’s Not Just a Suggestion
The expiration date isn’t there to push you to buy more. It’s the last day the drug is guaranteed to be safe and effective. Most prescriptions expire 12 to 18 months after they’re filled. After that, the medicine might not work as well. Some, like insulin or liquid antibiotics, can break down into harmful substances. Never take expired medication. If you’re not sure, bring it back to the pharmacy. They’ll dispose of it safely. Don’t flush it or toss it in the trash - that’s bad for the environment and dangerous if kids or pets get into it.
Prescription Number and Pharmacy Info
The Rx number is your prescription’s ID. It’s how the pharmacy tracks refills and links your bottle to your medical record. If you call for a refill and they ask for your Rx number, that’s why. The pharmacy’s name, phone number, and address are there so you can call with questions. Don’t ignore this. If you’re unsure how to take the medicine, call them. Pharmacists are trained to explain this stuff. They can also tell you if your medication interacts with other drugs you’re taking. And don’t forget the prescriber’s name - that’s your doctor or nurse practitioner. If something goes wrong, you need to know who to contact.
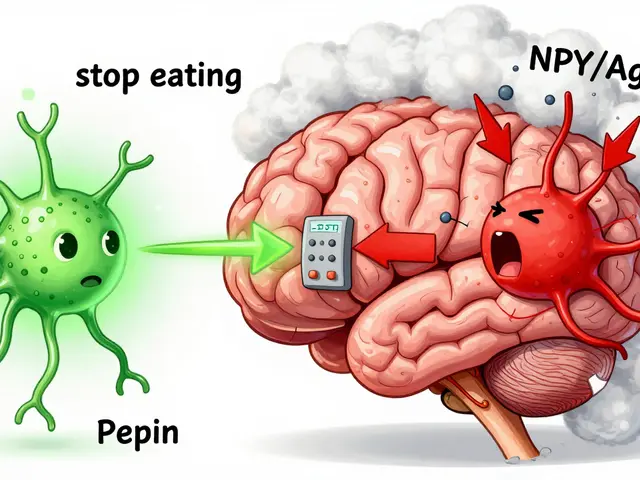
What Does the Medicine Even Do?
This is the part most labels still leave out - and it’s the biggest problem. Why were you given this pill? Is it for high blood pressure? For anxiety? For infection? If you don’t know the reason, you might take it when you shouldn’t. A 2020 FDA study found that 78% of patients took their meds wrong because they didn’t know why they were prescribed them. Some pharmacies now add the indication - like ‘for hypertension’ or ‘for thyroid replacement’ - right on the label. If yours doesn’t, ask. It’s not extra. It’s essential. Studies show adding the reason cuts wrong-drug errors by 55%. That’s huge. You’re not just taking a pill - you’re treating a condition. Know which one.
Appearance: Color, Shape, Imprint
Ever looked at your pill and thought, ‘This doesn’t look right’? That’s normal. Pills change shape, color, or size when you switch pharmacies or get a generic version. The label should describe it: ‘white, round, scored tablet with ‘50’ imprinted on one side.’ That’s your levothyroxine. If the pill looks completely different - say, blue instead of white, or oval instead of round - check the generic name. If it matches, it’s fine. If it doesn’t, or if the imprint is missing, call the pharmacy. A wrong pill can be deadly. Visual cues matter. That’s why USP recommends including this info - and why the FDA says it reduces confusion.
NDC Number - The Drug’s Social Security Number
You’ll see a long string of numbers: something like 00026-0225-01. That’s the National Drug Code (NDC). It’s unique to your exact medication - the manufacturer, the strength, even the bottle size. Pharmacists use it to order refills and track recalls. You don’t need to memorize it, but if there’s a recall - like a batch of metformin found to have a cancer-causing chemical - your pharmacy will use the NDC to know if your bottle is affected. Keep your labels until you finish the prescription. You might need that number later.
Storage Instructions - Keep It Safe
Some meds need to be kept cold. Others must stay dry. The label might say: ‘Store at room temperature, 68°-77°F’ or ‘Refrigerate.’ Don’t leave insulin in your hot car. Don’t keep antibiotics in the bathroom where steam and moisture can ruin them. Some pills break down faster in heat or humidity. If you’re unsure, ask the pharmacist. The right storage keeps your medicine working - and safe.

Warnings - Don’t Skip This Part
This is where the label gets serious. It might say: ‘Avoid alcohol,’ ‘May cause dizziness,’ ‘Do not use if pregnant,’ or ‘Risk of severe liver injury.’ These aren’t just fine print. They’re life-or-death. For example, mixing certain painkillers with alcohol can cause liver failure. Some meds make you so dizzy you can’t drive. If you have kidney disease, diabetes, or are over 65, warnings might be extra important. If you see a warning you don’t understand, ask. Don’t assume it doesn’t apply to you. The FDA says these warnings prevent thousands of hospitalizations every year.
What You Should Do Every Time You Get a New Prescription
Don’t just walk out with your bottle. Take two minutes. Ask yourself these five questions:
- What’s the name of this medicine - brand and generic?
- Why am I taking it? (If it’s not on the label, ask.)
- How much do I take, and when? (Write it down if you need to.)
- What side effects should I watch for?
- Does this interact with anything else I take - vitamins, alcohol, other meds?
Pharmacists are trained to answer these. Most will spend over two minutes explaining your meds. If they don’t, ask again. You’re not being difficult - you’re being smart.
What If the Label Still Doesn’t Make Sense?
If you’re still confused - or if you have trouble reading small print - ask for help. Many pharmacies now offer large-print labels or pictograms. Some even give you a QR code that links to a video explaining how to take the drug. If you’re not comfortable with English, ask for a label in your language. Federal law requires it. You have a right to understand your medicine. Don’t be shy. The goal isn’t to make you an expert - it’s to keep you safe.
Why This Matters More Than You Think
Medication errors don’t just cause stomach aches. They send 7,000 people to their graves every year in the U.S. - more than car accidents. Most of those errors are preventable. A clear label, a simple explanation, a quick question - those things save lives. You don’t need a medical degree to read your prescription label. You just need to pay attention. And if something doesn’t feel right? Trust your gut. Call the pharmacy. Ask your doctor. You’re not being a bother. You’re being responsible.
What if my prescription label doesn’t say why I’m taking the medicine?
If the reason for the medication isn’t listed, ask your pharmacist or doctor to add it. Many pharmacies now include this - it’s called the indication. Studies show that when patients know why they’re taking a drug, they’re 55% less likely to take it incorrectly. If your pharmacy doesn’t do it yet, request it. You have the right to understand your treatment.
Can I take a medicine after its expiration date?
It’s not recommended. Most medications lose effectiveness after expiration, and some - like insulin, liquid antibiotics, or nitroglycerin - can become dangerous. The FDA says expired drugs aren’t necessarily toxic, but you can’t be sure they’ll work. If you’re unsure, bring it to the pharmacy. They’ll dispose of it safely. Never take expired medicine, especially for serious conditions like heart disease or infection.
Why does my pill look different this time?
It’s likely a generic version from a different manufacturer. Generic drugs have the same active ingredient as the brand name, but they can look different in color, shape, or size. Always check the generic name on the label - if it matches what your doctor prescribed, it’s safe. If the name is different or you’re unsure, call the pharmacy before taking it.
Do I need to keep my prescription labels?
Yes, until you finish the bottle. The label has your Rx number, NDC code, and expiration date - all useful if you have side effects, need a refill, or are seeing a new doctor. If you’re concerned about privacy, you can cut off your name and phone number, but keep the drug name and dosage info. It helps you track what you’ve taken and when.
Can I get my prescription label in a bigger font or another language?
Yes. Under federal guidelines, pharmacies must provide labels in plain language and large print upon request. They’re also required to offer translations in the most common languages in their area - like Spanish, Mandarin, or Samoan. If you have trouble reading small text or don’t speak English well, ask. You’re not asking for a favor - you’re exercising your right to safe care.










Cindy Lopez
Label says 'take with food' - so I ate a bag of chips and called it a meal. Guess what? Still got sick. Thanks, pharmacy.
Ignacio Pacheco
So let me get this straight - the government mandates we read tiny print on a strip of paper to avoid dying, but won’t make the font bigger? Brilliant. Next they’ll tell us to meditate our way out of antibiotic resistance.
Katherine Gianelli
I used to ignore my labels too - until my grandma took the wrong pill and ended up in the ER. Now I read every word, even the tiny ones. I even write the reason I’m taking it on a sticky note and stick it to my mirror. It’s not fancy, but it keeps me alive. You don’t need a degree to be smart about your meds - just a little patience.
Jim Schultz
Oh wow, a 12-page essay on how to read a label?! Who knew this was a national crisis? I mean, seriously - if you can’t tell the difference between '10 mg' and '100 mcg', maybe you shouldn’t be allowed to own a pill organizer. Or a phone. Or a brain. This isn't education - it's damage control for people who think 'as needed' means 'whenever I feel like it'.
Joykrishna Banerjee
Let’s be honest: 90% of these ‘medication errors’ occur because patients are too lazy to Google their drug. The FDA doesn’t need to print more labels - they need to enforce basic literacy. Also, ‘NDC number’? That’s not a social security number - it’s a barcode. Stop anthropomorphizing pharmaceutical logistics.
Gavin Boyne
It’s funny how we treat medicine like a magic spell you get from a wizard in a white coat - then act shocked when it doesn’t work. The label isn’t a suggestion. It’s a contract. Between you, your doctor, the FDA, and the universe. Break it? You’re not just risking your health - you’re breaking the social contract of modern healthcare.
Francine Phillips
My label says ‘for hypertension’ now. I didn’t ask. They just added it. Feels weird knowing why I’m taking this little white thing. Like the pill finally made sense.
Kara Bysterbusch
As someone who grew up in a household where medicine was passed down like heirlooms - ‘This one’s for headaches, this one’s for nerves, this one’s from Aunt Linda’s trip to Mexico’ - I can’t emphasize enough how vital this clarity is. I remember my mother taking her neighbor’s blood pressure pills because they looked ‘similar.’ She didn’t die, but she almost did. This isn’t just information - it’s cultural repair. We need to stop treating medication like folklore. It’s science. And science deserves precision.
When I moved to the U.S., I was terrified of the pharmacy system. The labels were in English, the doses were in milligrams, and the warnings were in small caps. I didn’t know if I was being poisoned or protected. It took three visits and one patient advocate to make me feel safe. Now I help new immigrants read their labels. It’s not charity - it’s justice. You don’t need to speak perfect English to deserve to live.
And yes - I’ve asked for large-print labels. I’ve asked for Spanish translations. I’ve asked for QR codes. Every time, they said yes. Because in this country, when you ask for your right to health, they can’t legally say no. That’s something to hold onto.
So when you see someone standing at the counter, squinting at their bottle, don’t roll your eyes. Offer to read it with them. It takes two minutes. And two minutes might be the difference between a life and a statistic.
Pharmacists aren’t just dispensers. They’re translators. They’re teachers. They’re the last line between confusion and safety. Treat them like the experts they are - because they’re the only ones who know what’s really in that bottle.
Albert Essel
I used to think the expiration date was a marketing tactic - until I found a 10-year-old bottle of amoxicillin in my basement. I didn’t take it. But I also didn’t flush it. I took it to the pharmacy’s drug take-back bin. They thanked me. That’s the kind of small, responsible act we should celebrate - not shame. We’re not just consumers. We’re stewards of our own health.
Charles Moore
My dad had dementia. He’d take his pills at breakfast, lunch, and dinner - even if the label said ‘once daily.’ We tried pill boxes, alarms, charts - nothing worked. Then the pharmacy started putting a simple picture on the label: a sun for morning, a moon for night. He started taking them right. No one had thought to try that before. Sometimes the most powerful medicine isn’t in the pill - it’s in the design.
Myson Jones
As a pharmacy tech for 12 years, I’ve seen it all. People arguing because their generic pill is blue instead of yellow. People taking antibiotics until they feel better - then saving the rest for next time. People crying because they can’t afford their meds and don’t know how to ask for help. The label isn’t the problem. The system is. But reading it? That’s the first step toward changing it.
parth pandya
my label said take 1 pill 2x a day but i took 2 pills 2x a day cause i thought it meant 2 pills each time. i felt fine so i kept going. then i got dizzy and went to er. now i read the label. dumb mistake but live to tell it.
Chloe Madison
Every time I get a new prescription, I take a picture of the label and send it to my sister. She’s a nurse. She says ‘looks good’ and I breathe easier. You don’t have to be alone in this. Find your person. Someone who’ll read the fine print with you. That’s how we keep each other safe.
Kidar Saleh
In my village in Ghana, we used to crush herbs and boil them in pots. We didn’t have labels. We had elders. We had tradition. But here? We have this - a tiny strip of paper that holds the weight of modern medicine. And yet, we treat it like junk mail. We must honor it. Not because it’s legal. But because it’s sacred. It’s the bridge between science and survival.