Running out of your daily medication shouldn’t mean driving across town every month. If you’re taking pills for high blood pressure, diabetes, cholesterol, or depression, you’re not alone-millions of people do this. But here’s the truth: 90-day prescription supplies aren’t just a convenience. They cut down on trips, save money, and actually help you stay on track with your treatment. And yes, you can get one. You just need to know how to ask.
Why 90-Day Supplies Work Better Than Monthly
Most people get their prescriptions filled every 30 days. That’s four trips a year. But a 90-day supply? That’s just four trips a year. Less time in the pharmacy, less chance of forgetting, and fewer missed doses. Studies show people who get 90-day supplies are 27% more likely to take their meds as prescribed. That’s not a small boost-it’s the difference between your condition staying under control or flaring up. The math is simple: if you’re on a $100-a-month drug, a 30-day supply costs $100. A 90-day supply? Often $270 or less. That’s not a discount-it’s a 30% drop in out-of-pocket costs per month. For generics, it’s even better. Walmart, for example, charges $10 for a 90-day supply of common generic meds like metformin or lisinopril. That’s $3.33 a month. You’re not just saving time-you’re saving hundreds a year.Which Medications Qualify?
Not every drug is eligible. 90-day supplies are meant for maintenance medications-drugs you take daily for long-term conditions. Think:- High blood pressure (lisinopril, amlodipine)
- Diabetes (metformin, glimepiride)
- Cholesterol (atorvastatin, rosuvastatin)
- Depression and anxiety (sertraline, escitalopram)
- Thyroid (levothyroxine)
Drugs you take for a week or two? Not eligible. Antibiotics, painkillers after surgery, or short-term steroids don’t count. Even some drugs like oral contraceptives might only be available as 84-day supplies (three packs), but they still count as 90-day prescriptions under most plans.
Specialty drugs-like those for MS, rheumatoid arthritis, or cancer-are trickier. Most plans require you to fill a 30-day supply three times before you can switch to 90 days. That’s a rule, not a suggestion.
How to Get Started: 4 Simple Steps
Step 1: Check your insurance planLog into your insurer’s website or call the number on your card. Ask: “Do you offer 90-day supplies for maintenance meds?” Look for programs like Cigna 90 NowSM, Express Scripts, or CVS Caremark Mail Service. Medicare Part D plans must offer this option. Medicare Advantage plans sometimes go even further-Aetna, for example, offers 100-day supplies for its members. Step 2: Confirm your meds qualify
Open your medication list. Are you taking any of the maintenance drugs listed above? If yes, you’re likely eligible. If you’re unsure, call your pharmacy. They can tell you in seconds whether your prescription fits the criteria. Step 3: Talk to your doctor
This is where most people get stuck. Your doctor might default to writing a 30-day script. You need to ask for a 90-day supply. Say this: “I’d like to switch to a 90-day supply to make refills easier and save money. Is that possible?” Most doctors say yes. If they hesitate, mention that studies show better adherence with longer supplies. If they’re still unsure, ask them to check your insurer’s guidelines-they’re usually online. Step 4: Choose how you’ll get it
You have two main options:
- Mail order: Use your insurer’s mail pharmacy (like Express Scripts or CVS Caremark). You’ll get your meds delivered in 7-10 business days. This works best if you’re on a regular schedule and don’t need meds urgently.
- Pharmacy pickup: Some retail chains like Walmart, CVS, and Walgreens offer 90-day fills at the counter. Walmart is the cheapest for generics. Just bring your new prescription and ask for the 90-day option. No mail needed.
Important: If you’re on Cigna 90 NowSM, you can’t just go to any pharmacy. You must use one in their network. Check their website first. Same goes for Express Scripts-only certain pharmacies are approved.
What Could Go Wrong (And How to Fix It)
You might hit a snag. Here’s what to expect:- Your doctor won’t write a 90-day script. Don’t take no for an answer. Ask if they can use an electronic system to send it to your mail pharmacy. Many insurers have tools that make this easy for doctors. Or ask the pharmacy to call the doctor on your behalf.
- Your pharmacy says it’s not allowed. Double-check your plan. Some states block 90-day programs-California, Minnesota, New Hampshire, Texas, and Washington have restrictions. If you live there, mail order might be your only option.
- You’re on a specialty drug. You’ll need three 30-day fills first. Keep the receipts. Once you’ve done that, call your pharmacy and ask to switch.
- The cost is higher than expected. Check your tier. Brand-name drugs cost more than generics. If you’re paying $40 for a 90-day supply, ask if a generic version exists. If it does, your doctor can switch you.
What to Do After You Get Your 90-Day Supply
Once you have it, set up reminders. Most mail-order pharmacies send texts or emails when your refill is due. Sign up for them. Use your insurer’s app-Cigna, CVS, and Express Scripts all have dashboards where you can track your meds, reorder, and see your spending. Also, keep your original 30-day script until your 90-day supply arrives. Don’t run out. If you’re switching from retail to mail, give yourself a 10-day buffer. That way, you never go without.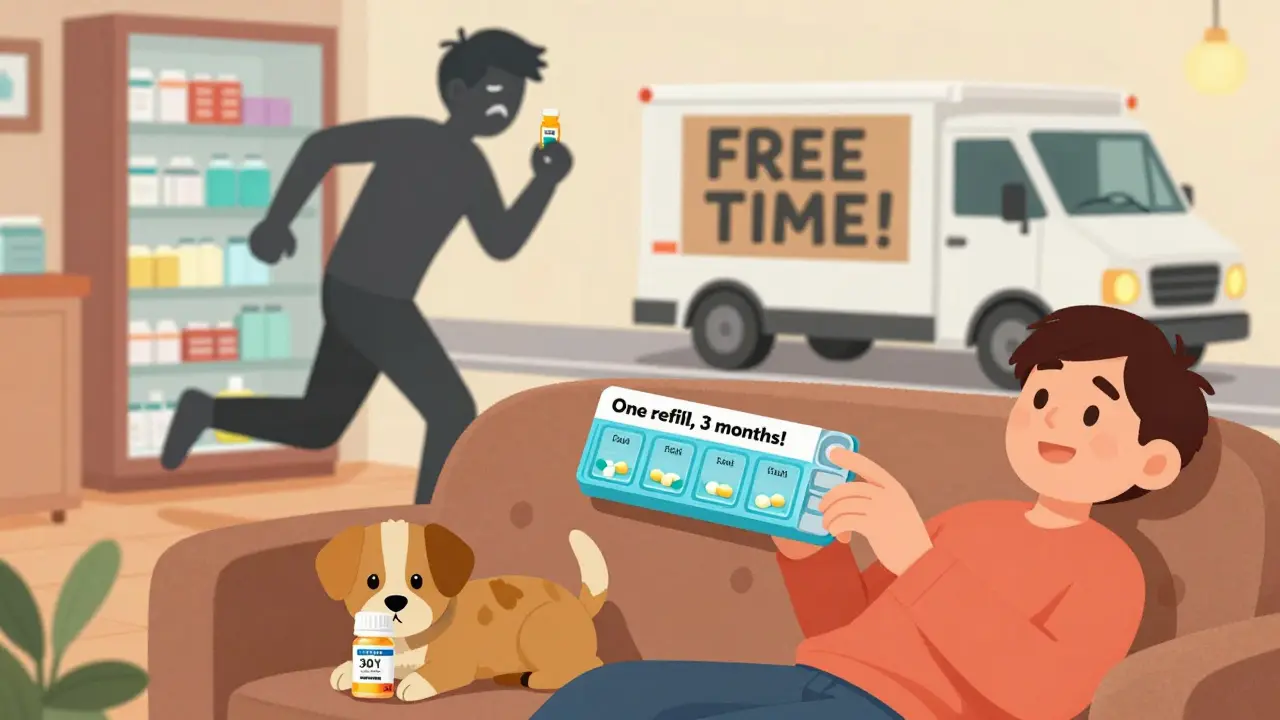
Who Can’t Use This? (And What They Can Do)
Medicare and Medicaid beneficiaries in some states can’t use certain 90-day programs. If you’re in California or Texas, your options are limited. But you can still get 90-day supplies through mail-order pharmacies approved by Medicare Part D. Call 1-800-MEDICARE to ask which ones are available in your area. If you’re uninsured, Walmart, Target, and Costco offer ultra-low prices on generics. A 90-day supply of metformin? $10. That’s cheaper than most insurance copays.Final Thought: It’s Not About Convenience-It’s About Your Health
Skipping doses because you forgot to refill? That’s not laziness. It’s a system failure. The pharmacy system was built for 30-day fills. But your body doesn’t care about that. It needs consistency. A 90-day supply removes the friction. Less stress. Fewer missed days. Better control. And yes-less time in the parking lot of the pharmacy. You don’t need to be a medical expert to ask for this. You just need to know it’s an option. And now you do.Can I get a 90-day supply for any medication?
No. Only maintenance medications for chronic conditions qualify-like those for high blood pressure, diabetes, cholesterol, or depression. Short-term drugs like antibiotics, painkillers, or steroids don’t qualify. Specialty drugs usually require three 30-day fills before you can switch to 90 days.
Do I need a new prescription for a 90-day supply?
Yes. Your doctor must write a new prescription for 90 days. You can’t just ask the pharmacy to extend your existing 30-day script. The prescription must specify the quantity (e.g., 90 tablets) and days’ supply (90 days). Most doctors can send this electronically to a mail pharmacy or your local pharmacy.
Is a 90-day supply cheaper than three 30-day fills?
Almost always. Even if your copay is the same per fill, insurers often lower the cost for 90-day supplies. For example, a 30-day generic might cost $15, so three fills would be $45. A 90-day supply might cost $25-$30. Walmart offers many generics at $10 for 90 days. You’re saving money and time.
Can I use my local pharmacy for a 90-day supply?
Yes-if your plan allows it. Some insurers like Cigna restrict 90-day fills to select network pharmacies. Others, like Walmart, let you get it right at the counter. Check your plan’s website or call customer service. If your local pharmacy says no, ask if they can order it through your insurer’s mail service.
What if I live in a state that doesn’t allow 90-day supplies?
States like California, Minnesota, New Hampshire, Texas, and Washington have restrictions on certain 90-day programs. But Medicare Part D plans still offer mail-order 90-day supplies in these states. Call 1-800-MEDICARE to find approved pharmacies. If you’re uninsured, pharmacies like Walmart and Costco still offer low-cost generic 90-day supplies regardless of your state.











Freddy King
Let’s be real-the 90-day supply thing is just pharmacy logistics dressed up as a health hack. You’re not ‘saving money,’ you’re just shifting the cost structure to bulk purchasing. The 27% adherence boost? Correlation isn’t causation. People who care enough to ask for 90-day scripts are probably the same ones who already take their meds. The system rewards the conscientious, not the struggling.
And don’t get me started on Walmart’s $10 metformin. That’s not a discount-it’s a subsidy. The real cost is hidden in your premiums. You think you’re winning? You’re just not seeing the full balance sheet.
Also, ‘maintenance meds’ is such a corporate euphemism. It makes chronic illness sound like a subscription service. You’re not maintaining, you’re surviving. But hey, if it gets you out of the parking lot faster, I guess that’s progress.