Autoimmune Disease: What It Is and How to Manage It
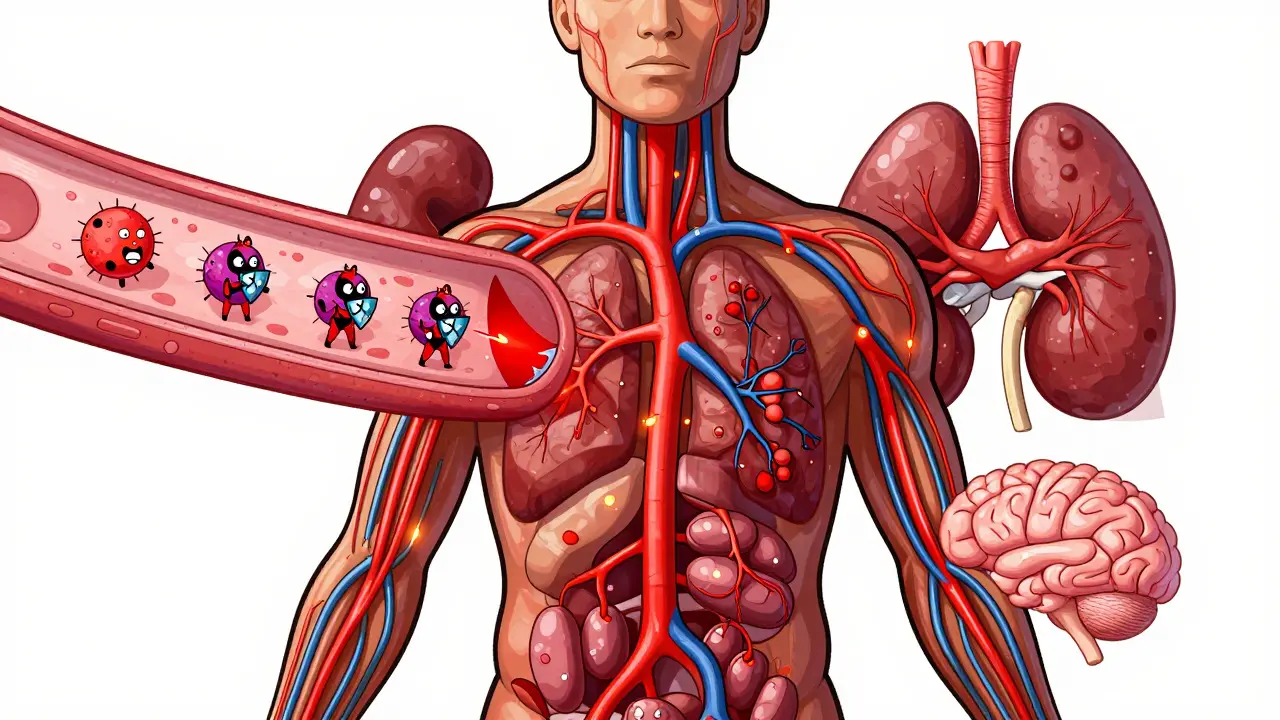
If your body’s immune system seems to be fighting you instead of protecting you, you might be dealing with an autoimmune disease. These conditions happen when the immune system mistakenly attacks healthy tissue, leading to pain, fatigue, or organ damage. The good news is that many people learn to live well with them by understanding the signs and getting the right care.
Spotting the Common Symptoms
Autoimmune disorders don’t all look the same, but a few red flags show up over and over. Persistent fatigue that doesn’t improve with sleep is one of the most common clues. Joint pain or swelling—especially if it moves from joint to joint—is another sign you might see in rheumatoid arthritis or lupus.
Skin changes also give hints. Rashes that flare after sun exposure often point to lupus, while itchy patches can signal psoriasis. If you notice sudden weight changes, hair loss, or trouble concentrating (sometimes called "brain fog"), those could be related too.
The trick is to track what feels off and share it with your doctor. Even a vague symptom like “I feel sore all the time” can help narrow down which autoimmune condition you might have when combined with lab tests.
How Doctors Diagnose Autoimmune Conditions
Diagnosis usually starts with a detailed medical history and physical exam. Your doctor will ask about family history because genetics play a role in many autoimmune diseases. Blood tests are the next step—tests like ANA (antinuclear antibody) can flag lupus, while rheumatoid factor helps spot rheumatoid arthritis.
Imaging studies such as X‑rays or MRIs may be ordered to see how much joint damage has occurred. In some cases, a biopsy of skin or organ tissue gives the clearest picture.
Don’t be surprised if it takes a few appointments to get a final answer. Autoimmune diseases can overlap, and doctors often need to rule out other causes first.
Everyday Ways to Keep Symptoms in Check
While medication is a cornerstone of treatment, lifestyle tweaks make a big difference. Prioritize sleep—most adults need 7‑9 hours per night, and poor rest can worsen inflammation.
Eating a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats helps control flare-ups. Some people find that cutting out processed foods, sugar, or gluten reduces symptoms, but keep a food journal to see what works for you.
Gentle exercise like walking, swimming, or yoga keeps joints flexible and can lift mood‑boosting hormones. Start slow and listen to your body; overdoing it can trigger a flare.
Stress management is also key. Techniques such as deep breathing, meditation, or simply taking short breaks during the day have been shown to lower cortisol levels, which in turn may calm an overactive immune response.
Treatment Options You’ll Hear About
Doctors often start with non‑steroidal anti‑inflammatory drugs (NSAIDs) for mild pain. If symptoms are more severe, disease‑modifying antirheumatic drugs (DMARDs) like methotrexate can slow the immune attack.
Biologic therapies—injectable medications that target specific parts of the immune system—are common for conditions such as rheumatoid arthritis and psoriasis. They’re powerful but require careful monitoring.
Corticosteroids provide fast relief during flare‑ups, but long‑term use isn’t ideal because of side effects like weight gain or bone loss.
In recent years, newer oral small‑molecule drugs have entered the market, offering another way to tame immune activity without injections. Talk with your rheumatologist or immunologist about which option fits your situation best.
When to Seek Professional Help
If you notice new or worsening symptoms—especially sudden organ pain, severe fatigue, or unexplained fevers—call your doctor right away. Early intervention can prevent irreversible damage.
Regular check‑ups are essential even when you feel fine. Blood work every few months helps track disease activity and adjust medication doses before a flare hits.
Support groups, whether online or in person, also provide practical tips and emotional encouragement. Sharing experiences with others who get it can make managing an autoimmune disease less isolating.
Living with an autoimmune condition is a marathon, not a sprint. By recognizing symptoms early, staying on top of medical care, and making smart lifestyle choices, you can keep the immune system in check and enjoy everyday life.