Portal Hypertension: Causes, Risks, and What You Need to Know
When blood can't flow freely through the portal hypertension, a condition where blood pressure rises in the portal vein that carries blood from the intestines to the liver. It's not a disease on its own—it's a warning sign your liver is damaged. This isn't just about numbers on a chart. It's about your body struggling to process nutrients, filter toxins, and manage fluid. Left unchecked, it leads to dangerous complications like swollen veins in your esophagus, fluid buildup in your belly, and even life-threatening bleeding.
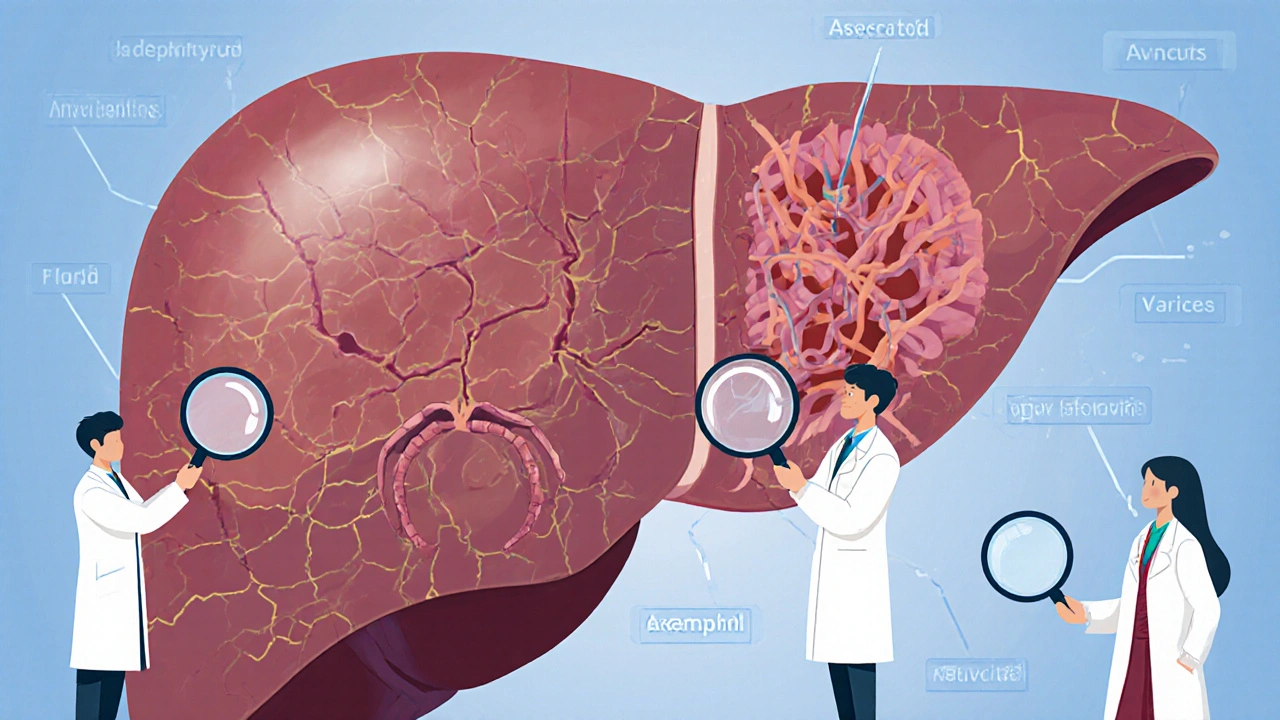
Most cases of portal hypertension, a condition where blood pressure rises in the portal vein that carries blood from the intestines to the liver. It's not a disease on its own—it's a warning sign your liver is damaged come from cirrhosis, scarring of the liver that blocks normal blood flow. Alcohol, hepatitis, fatty liver disease—these all wear down your liver over time. As scar tissue builds up, the portal vein gets squeezed. Blood backs up. Pressure climbs. That’s when you start seeing symptoms: a bloated belly from ascites, fluid leaking into the abdominal cavity due to increased pressure, swollen veins in your throat or stomach called varices, enlarged, fragile veins that can rupture and bleed, or even confusion from toxins your liver can’t clear anymore.
What’s scary is that many people don’t feel anything until something serious happens—a sudden bleed, extreme swelling, or a drop in alertness. That’s why knowing your risk matters. If you’ve been told you have fatty liver, drink regularly, or have had hepatitis, don’t wait for symptoms. Get checked. Simple tests like ultrasound or blood work can spot early signs. And if you’re already diagnosed, managing it isn’t just about medication—it’s about diet, avoiding alcohol, and working with your doctor to monitor pressure and prevent complications.
The posts below cover real-world connections to portal hypertension: how certain diabetes drugs affect liver health, what pain meds to avoid when your liver is under stress, how fluid buildup is managed, and why some antibiotics or antifungals need careful monitoring in people with liver disease. You’ll find practical advice on medication safety, dietary tips, and warning signs you can’t ignore. This isn’t theoretical—it’s about protecting your body before it’s too late.
Cirrhosis is the advanced stage of chronic liver disease, marked by scarring and declining function. Learn about its major complications-ascites, bleeding, brain fog, and cancer-and how to manage them with diet, meds, and monitoring.