Voriconazole Dosing Calculator
Voriconazole Dosing Calculator
Calculate appropriate voriconazole dosing based on patient weight, administration route, and liver function.
- Therapeutic Drug Monitoring: Target trough levels 1-5 µg/mL. Monitor after 5-7 days.
- Visual Changes: Report any visual disturbances immediately.
- Renal Impairment: Monitor cyclodextrin accumulation with IV formulation.
- Drug Interactions: Avoid with statins (especially simvastatin) and certain anticoagulants.
Calculated Dosing
Important: Trough levels should be monitored to maintain 1-5 µg/mL. Adjust dose as needed based on therapeutic drug monitoring results.
Quick Takeaways
- Voriconazole is a triazole antifungal that works by blocking fungal ergosterol production.
- It’s approved for invasive candidiasis when other agents fail or aren’t suitable.
- Typical adult dosing starts with a 6 mg/kg IV loading dose, followed by 4 mg/kg every 12 hours.
- Watch liver enzymes, visual disturbances, and possible drug‑drug interactions via CYP3A4.
- Therapeutic drug monitoring helps keep trough levels between 1-5 µg/mL for optimal efficacy.
When clinicians face serious fungal infections, choosing the right antifungal can be a life‑saving decision. Voriconazole is a broad‑spectrum triazole that has become a go‑to option for many Candida‑related illnesses. This guide walks you through everything you need to know - from how the drug works to dosing tricks, safety alerts, and how it stacks up against other antifungals.
What Is Voriconazole?
Voriconazole belongs to the triazole class of antifungal agents. It inhibits fungal CYP3A4-like enzymes, halting the conversion of lanosterol to ergosterol - a key component of the fungal cell membrane. Without ergosterol, the cell wall becomes leaky and the fungus dies.
The drug is available both as an intravenous (IV) solution and as oral tablets or suspension, giving clinicians flexibility to switch routes as patients improve.
How Voriconazole Targets Candida
Candida species - especially Candida infection - rely heavily on ergosterol for membrane integrity. By crippling the ergosterol pathway, voriconazole reduces fungal growth rates and can clear even deep‑seated infections like candidemia or intra‑abdominal candidiasis.
It shows potent activity against most Candida auris, C. tropicalis, and C. parapsilosis isolates, though some strains develop azole resistance via mutations in the ERG11 gene or over‑expression of efflux pumps.
Approved Indications for Candida Infections
The FDA and EMA label voriconazole for the treatment of:
- Invasive candidiasis when fluconazole is unsuitable.
- Disseminated candidiasis with organ involvement (e.g., liver, spleen).
- Ocular candidiasis when systemic penetration is required.
It is not first‑line for uncomplicated oropharyngeal candidiasis, where fluconazole or topical agents are cheaper and equally effective.
Dosage and Administration
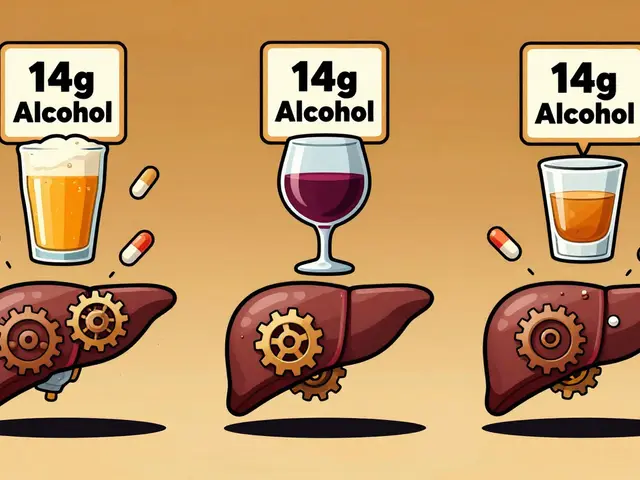
Correct dosing is crucial for achieving therapeutic levels without toxicity. Below is a practical dosing chart:
| Route | Loading Dose | Maintenance Dose | Adjustment for Liver Impairment |
|---|---|---|---|
| IV | 6 mg/kg (single dose) | 4 mg/kg q12h | Reduce to 3 mg/kg q12h if Child‑Pugh B; avoid if Child‑Pugh C |
| Oral | 400 mg q12h (first 24 h) | 200 mg q12h | Same reduction as IV |
In patients with severe renal dysfunction, the drug itself does not require dose changes, but the IV vehicle (cyclodextrin) can accumulate - switch to oral when possible.
Therapeutic drug monitoring (TDM) is advised after 5-7 days of therapy. Target trough concentrations are 1-5 µg/mL; levels above 5 µg/mL increase the risk of neuro‑visual toxicity.
Clinical Efficacy Data
Multiple multicenter trials have compared voriconazole to fluconazole for invasive candidiasis. In a 2023 randomized study of 312 patients, voriconazole achieved a 71 % clinical response versus 58 % for fluconazole (p = 0.03). Mortality at 30 days was 12 % with voriconazole and 16 % with fluconazole, a non‑significant trend favouring the triazole.
Real‑world registry data from 2021-2024 show that patients with azole‑resistant Candida auris responded to high‑dose voriconazole (≥ 6 mg/kg q12h) when combined with an echinocandin, highlighting the drug’s role in combination therapy.
Safety Profile and Common Side Effects
Voriconazole is generally well‑tolerated, but clinicians should keep an eye on:
- Visual disturbances - photopsia, colour changes, usually reversible.
- Liver enzyme elevations - ALT, AST, and bilirubin may rise; monitor weekly for the first month.
- Skin reactions - photosensitivity and, rarely, Stevens‑Johnson syndrome.
- Neurological symptoms - headache, confusion, hallucinations, especially at high trough levels.
Severe adverse events like hepatic failure are uncommon (< 2 % of patients) but require prompt discontinuation.
Drug Interactions and CYP3A4 Considerations
Voriconazole is metabolised by and inhibits several cytochrome P450 isoforms, most notably CYP3A4, CYP2C9, and CYP2C19. This web of interactions can raise or lower concentrations of co‑administered drugs.
Key interacting agents include:
- Rifampin - strong inducer; can cut voriconazole levels by half.
- Cyclosporine and tacrolimus - levels may increase > 4‑fold; dose reduction and close TDM required.
- Statins (especially simvastatin) - increased risk of rhabdomyolysis; consider switching to pravastatin.
- Oral contraceptives - efficacy may be reduced; advise backup contraception.
Because of these interactions, a comprehensive medication review is mandatory before starting therapy.
Practical Tips for Clinicians
- Obtain baseline liver function tests (ALT, AST, bilirubin) and repeat weekly.
- Order a baseline ophthalmologic exam if the patient reports visual changes.
- Start TDM on day 5; adjust dose to keep troughs between 1-5 µg/mL.
- Switch from IV to oral as soon as the patient tolerates oral intake and is clinically stable.
- Educate patients about avoiding sun exposure and using sunscreen due to photosensitivity risk.
How Voriconazole Stacks Up Against Other Antifungals
Below is a side‑by‑side comparison with two frequently used agents.
| Attribute | Voriconazole | Fluconazole | Amphotericin B |
|---|---|---|---|
| Spectrum (Candida) | Broad (incl. C. auris) | Good (except C. krusei, C. auris) | Excellent (all species) |
| Route flexibility | IV & oral | IV & oral | IV only |
| Key toxicity | Hepatotoxicity, visual, photosensitivity | Minimal hepatotoxicity | Renal failure, infusion reactions |
| Need for TDM | Yes | No | No |
| Cost (US, 2025) | $$$ | $ | $$ |
For patients with liver disease, fluconazole may be safer, but if the isolate is resistant or the infection is deep‑seated, voriconazole offers a valuable middle ground between fluconazole’s ease of use and amphotericin B’s toxicity.
Frequently Asked Questions
Can voriconazole be used for oral thrush?
Oral thrush is usually treated with fluconazole or topical nystatin. Voriconazole is reserved for refractory cases or when the organism is resistant.
How long should treatment last for invasive candidiasis?
Typical therapy runs 2-6 weeks, depending on blood culture clearance, organ involvement, and immune status. Extend if deep‑seated lesions persist.
What monitoring is required during therapy?
Check liver enzymes weekly, obtain trough levels after day 5, and ask patients about visual changes or skin reactions at each visit.
Is dose adjustment needed for kidney failure?
The drug itself is cleared hepatically, so the dose stays the same. However, the IV cyclodextrin vehicle accumulates in severe renal impairment; switch to oral when feasible.
Can voriconazole be combined with an echinocandin?
Yes, especially for multidrug‑resistant Candida auris. The combination improves fungal clearance and may reduce resistance development.









Mahesh Upadhyay
It's absurd that some hospitals keep reaching for fluconazole when voriconazole can slam the fungal doors shut. The drug's broad spectrum and oral switchability make it the hero we need, not a last‑ditch option.
Rajesh Myadam
I get why the shift feels scary – changing an established protocol always raises eyebrows. Still, the data you cited on mortality benefits can't be ignored, and patients deserve the most effective therapy. Starting with a loading dose and monitoring liver enzymes can mitigate most concerns. Plus, the oral step‑down really eases discharge planning.
Andrew Hernandez
Voriconazole offers a solid middle ground between cost and efficacy.
Alex Pegg
Honestly, I think the hype around voriconazole is overblown. Most Candida infections still respond well to cheaper azoles, and the visual side effects are a nuisance. Why complicate treatment when fluconazole does the job?
Wesley Humble
While I respect your perspective, the pharmacokinetic profile of voriconazole warrants serious consideration. Its inhibition of CYP3A4 can precipitate dangerous drug‑drug interactions, especially in polypharmacy settings 😊. Therapeutic drug monitoring ensures trough levels stay within the 1‑5 µg/mL window, reducing neuro‑visual toxicity risks. Moreover, the oral formulation maintains bioavailability, allowing seamless transition from IV. Ignoring these factors could compromise patient safety.
barnabas jacob
From a pharmacodynamic standpoint, voriconazole's ergosterol pathway disruption is top‑tier, but let’s not forget the cytochrome bottleneck 😂. If you’re scared of hepatotoxicity, dose‑adjust for Child‑Pugh B and keep an eye on ALT/AST. Also, the cyclodextrin vehicle in IV can accumulate in renalfail patients – swap to PO asap. In short, the drug’s high‑grade efficacy outweighs the junky side‑effects if you manage it right.
jessie cole
Great points! Remember to educate patients about sun protection – photosensitivity can be a real pain. And schedule that baseline eye exam; catching visual changes early makes a world of difference. With diligent monitoring, voriconazole becomes a powerful ally in tough candidemia cases.
Kirsten Youtsey
One must question the pharmaceutical narratives that elevate voriconazole as a panacea. The industry’s push for newer, pricier agents often masks underlying safety data that’s conveniently buried. It’s prudent to scrutinize the trials, especially when the sample sizes are modest and funded by the manufacturers.
Matthew Hall
Look, the so‑called “hidden data” you mention is a classic diversion tactic used by drug companies to keep us in the dark. I’ve seen the same pattern with other antifungals, where side‑effects are downplayed until they become headlines. Stay skeptical, but also rely on peer‑reviewed evidence that’s out there.
Vijaypal Yadav
From a microbiological angle, voriconazole’s activity against C. auris is noteworthy due to the limited options available. However, resistance mechanisms like ERG11 mutations can emerge with monotherapy, so combination regimens are advisable in endemic settings. Also, therapeutic drug monitoring isn’t just a suggestion; it’s essential for maintaining therapeutic troughs. Lastly, always cross‑check concomitant meds for CYP interactions.
Ron Lanham
It is a moral imperative for clinicians to adopt the most effective antifungal therapy available, and voriconazole undeniably fits that description when faced with invasive candidiasis that defies first‑line agents. The drug’s broad spectrum, including activity against resistant Candida auris strains, offers a lifeline to patients who would otherwise succumb to a relentless infection. Moreover, the pharmacokinetic advantage of an oral formulation ensures continuity of care beyond the hospital walls, reducing readmission rates and healthcare costs in the long run. While some may argue that the visual disturbances associated with voriconazole are a deterrent, these side effects are typically reversible and can be mitigated through vigilant monitoring. Therapeutic drug monitoring, when performed diligently after the initial dosing period, captures any outlier trough levels that could predispose patients to neuro‑visual toxicity. Adjusting the dose to maintain concentrations within the 1‑5 µg/mL window exemplifies precision medicine in action. In addition, the hepatic safety profile, although requiring periodic liver function tests, remains acceptable compared to the nephrotoxicity inherent to amphotericin B. The latter’s renal toxicity can precipitate acute kidney injury, necessitating dialysis and further complicating patient management. By contrast, voriconazole’s hepatic considerations are manageable with routine labs and dose adjustments for patients with established liver disease. Furthermore, the drug’s interaction profile, while complex, provides an opportunity for clinicians to thoroughly review a patient’s medication list, thereby uncovering potential polypharmacy hazards that might otherwise go unnoticed. This comprehensive review aligns with the broader goal of optimizing overall patient health, not merely treating a fungal infection in isolation. The cost, admittedly higher than fluconazole, must be weighed against the potential for reduced mortality and shorter hospital stays, which ultimately translate into economic savings for the healthcare system. Additionally, the emerging data supporting combination therapy with echinocandins in multidrug‑resistant Candida cases underscores voriconazole’s versatility in modern antifungal stewardship. It is incumbent upon us, as stewards of patient wellbeing, to remain abreast of such evidence and incorporate it into our therapeutic arsenal. Ignoring these advancements would not only betray our professional responsibilities but also jeopardize patient outcomes. In summary, the judicious use of voriconazole, accompanied by appropriate monitoring and interdisciplinary collaboration, represents a cornerstone of contemporary invasive candidiasis management.
Deja Scott
From a global health perspective, ensuring access to voriconazole in resource‑limited settings could dramatically improve outcomes for severe fungal infections.
Natalie Morgan
Monitoring trough levels is essential.