A cerebral aneurysm isn’t something most people think about until it’s too late. But here’s the hard truth: about 3.2% of adults worldwide have one - often without knowing it. Most never rupture. But if one does, the chances of dying within the first day are between 30% and 40%. That’s why understanding your risk and knowing your options isn’t just helpful - it could save your life.
What Exactly Is a Cerebral Aneurysm?
A cerebral aneurysm is a weak spot in the wall of a brain artery that balloons out like a small bubble. Think of it as a thin patch on a garden hose that swells under pressure. Most stay small and never cause problems. But when that wall gives way, blood floods into the space around the brain - a condition called subarachnoid hemorrhage. This isn’t a minor bleed. It’s a medical emergency that can cause stroke, brain damage, or death.
The good news? Most aneurysms never rupture. The bad news? You can’t always tell which ones will. That’s why doctors look at more than just size. They look at shape, location, and even your lifestyle.
Who’s at Risk for Rupture?
Some risks you can’t change. Age is a big one. If you’re over 65, your rupture risk is 2.7 times higher than someone in their 40s. Women are more likely than men to develop aneurysms - about 1.6 times more often. And if two or more close family members had one, your risk jumps fourfold.
But the biggest risks? The ones you can control.
- Hypertension: If your systolic blood pressure is above 140 mmHg, your rupture risk goes up by 2.3 times.
- Smoking: Current smokers face a 3.1 times higher risk. If you smoke more than 10 cigarettes a day, that risk climbs another 47%.
- Alcohol: Drinking more than 14 drinks a week increases rupture risk by 32%.
These aren’t just numbers. They’re real, measurable dangers. Quitting smoking cuts your rupture risk by 54% in just two years. Lowering your blood pressure to under 130/80 mmHg isn’t just good for your heart - it’s critical for your brain.
Size, Shape, and Location Matter More Than You Think
It’s not just about how big the aneurysm is. A 7mm aneurysm has a hazard ratio of 3.1 for rupture compared to smaller ones. But shape? That’s even more telling. Irregular shapes - think lumpy, not round - carry a 2.9 times higher risk. And if there’s a smaller bulge sticking off the main sac (called a daughter sac), your risk jumps 68%.
Location is crucial, too. Aneurysms in the anterior communicating artery (AComm) are especially dangerous. They rupture more often than others, even when they’re under 5mm. Middle cerebral artery aneurysms have a 3.6 times higher rupture risk. Meanwhile, distal anterior cerebral artery aneurysms can burst at sizes most doctors would consider safe.
And if you have more than one aneurysm? Your risk multiplies. People with multiple aneurysms are 3.8 times more likely to have one rupture. If you’ve already had one rupture, your chance of another is 5.2 times higher.
The PHASES Score: Your Personal Rupture Risk Calculator
Doctors don’t guess when deciding if you need treatment. They use tools. The most trusted is the PHASES score. It’s based on six factors:
- Population (where you live)
- Hypertension
- Age
- Aneurysm size
- History of prior subarachnoid hemorrhage
- Location of the aneurysm
You get a score from 0 to 10. Each point adds up. A score of 0-3 means your 5-year rupture risk is only 3%. A score of 9-10? That’s a 45% chance. Most guidelines say if your PHASES score is 6 or higher, treatment should be considered.
There’s also the ELAPSS score and the triple-S model (size, site, shape), which help predict risk over shorter periods - like the next 6 or 12 months. These tools aren’t perfect, but they’re the best we have.
How Are Cerebral Aneurysms Treated?
There are three main ways to treat an aneurysm - and the right choice depends on your anatomy, age, and overall health.
1. Surgical Clipping
This is the oldest method, first done in 1937. A neurosurgeon opens the skull (craniotomy) and places a tiny titanium clip across the neck of the aneurysm, cutting off blood flow. It’s a major surgery, but it’s also the most permanent. About 95% of clipped aneurysms are completely sealed. Long-term, 88-92% stay closed for good.
But it’s not risk-free. Permanent complications happen in 4.7% of cases. Death occurs in 1.5%. And recovery takes weeks - sometimes months.
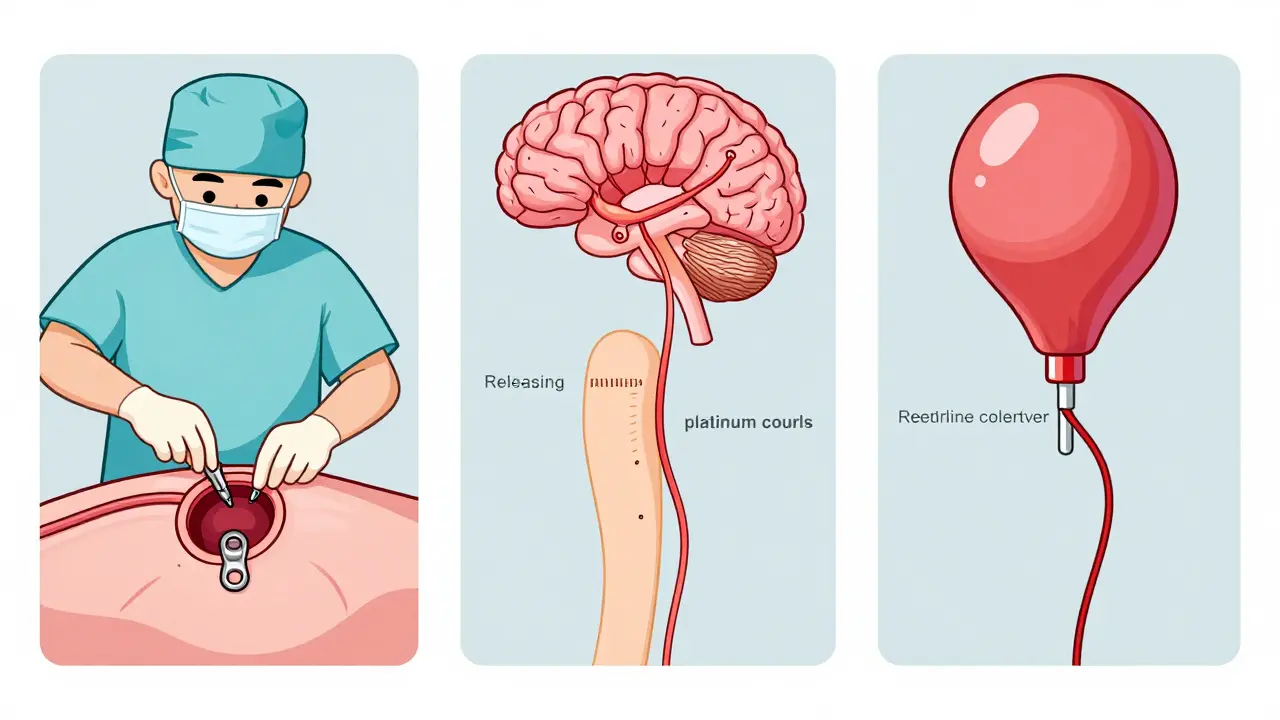
2. Endovascular Coiling
This is the less invasive option. A catheter is threaded from the groin up to the brain. Tiny platinum coils are released into the aneurysm, triggering a blood clot that seals it off. Success rates are 78-85% at 6 months.
The big advantage? Faster recovery. Most people go home in a day or two. Mortality is lower - 1.1%. Complication rates are also lower at 3.9%. But here’s the catch: you’re more likely to need a second procedure. About 15.7% of coiled aneurysms need retreatment over 12 years, compared to just 6.2% for clipped ones.
3. Flow Diversion
This is the newest option. A special stent - like the Pipeline Embolization Device - is placed in the artery. It doesn’t block the aneurysm directly. Instead, it redirects blood flow away from it. Over time, the aneurysm shrinks and disappears.
It works best for large or giant aneurysms, or those with wide necks that are hard to coil. Success rates hit 76.4% at 6 months, and newer versions like the PED-PLATINIUM show 85.5% occlusion at 1 year.
But it’s not for everyone. You need to take blood thinners for months after. And the complication rate is slightly higher - 5.2% permanent morbidity.
When Is Observation the Best Choice?
Not every aneurysm needs treatment. In fact, many don’t.
The UCAS Japan study found that for unruptured aneurysms smaller than 5mm, the 5-year rupture risk is just 0.2% for those in the front of the brain and 0.7% in the back. For low-risk patients - younger, no smoking, normal blood pressure, small size - watching and waiting with annual MRA scans is often the smartest move.
Doctors use PHASES and other scores to decide. If your risk is low, you avoid surgery. If your aneurysm grows over time, or your PHASES score climbs, then treatment becomes the clear next step.
What About New Treatments?
There’s exciting progress. The WEB (Woven EndoBridge) device is FDA-approved for aneurysms at artery branches (bifurcations). In trials, it achieved 71.4% complete occlusion at 1 year.
Researchers are also looking at genetic markers. The HUNT study found 17 gene locations linked to aneurysm formation and rupture. Machine learning models are now analyzing dozens of factors - shape, blood flow patterns, wall stress - to predict rupture better than any single score.
Long-Term Outcomes: What Happens After Treatment?
Successful treatment cuts your 10-year re-rupture risk from 68% down to just 2.3%.
Quality of life matters, too. People who had endovascular treatment reported better scores on quality-of-life tests (EQ-5D: 0.82 vs. 0.76 for surgery) at one year. That’s not just about physical recovery - it’s about returning to work, family life, and daily routines faster.
But long-term follow-up is essential. Even after clipping or coiling, you need regular imaging to make sure the aneurysm stays closed and no new ones form.
Bottom Line: What Should You Do?
If you’ve been told you have a cerebral aneurysm, don’t panic. But don’t ignore it either.
Ask your doctor:
- What’s my PHASES score?
- What’s the size, shape, and location of my aneurysm?
- Do I have other risk factors - smoking, high blood pressure, family history?
- Is observation safe for me right now?
- What are the risks and benefits of each treatment option?
And take control of what you can: quit smoking, get your blood pressure under control, cut back on alcohol. These steps alone can cut your risk by more than half.
A cerebral aneurysm isn’t a death sentence. It’s a warning - and with the right information, you can turn that warning into a second chance.











Simran Kaur
This hit me so hard. My mom had an unruptured aneurysm found during a routine scan-she was 58, non-smoker, BP under control. They watched it for 3 years. She’s alive today because she didn’t panic, and her doctor didn’t rush her. I wish more people knew it’s not always about cutting or coiling. Sometimes, it’s about breathing, waiting, and trusting the science.
Thank you for writing this. I’m sharing it with my entire family.
Neil Thorogood
So let me get this straight… if I smoke, drink, and have high blood pressure, I’m basically playing Russian roulette with my brain? 🤡
And the worst part? I’m 32. I still think I’m invincible. Guess I’m the 3.2% who doesn’t know they’re walking around with a ticking time bomb. Thanks for the wake-up call, doc. Now I gotta quit smoking. Again. 😅
Jessica Knuteson
PHASES score is just another metric to sell procedures. The real issue is the medical-industrial complex turning asymptomatic findings into crises. Most aneurysms never rupture. Most people die of other things anyway. Why are we pathologizing anatomy?
Observation isn’t neglect. It’s wisdom. The data proves it. The fear? That’s manufactured.
Robin Van Emous
I appreciate this breakdown. Really. But I’ve got to say-I’ve seen too many people get scared by a scan result and rush into surgery because they think ‘if it’s there, it must be fixed.’
It’s not that simple. My uncle had a 4mm aneurysm in his AComm. Low PHASES score. No smoking. Normal BP. They watched it. Ten years later? Still there. Still fine.
Don’t let fear make decisions for you. Talk to your neurologist. Ask for the numbers. And if they push you toward surgery without explaining the risk-benefit? Get a second opinion. Always.
Angie Thompson
OMG I just read this and my heart is racing 😭
I’m 29, had a migraine last year that scared me so bad I got an MRI-and they found a 3mm aneurysm. I’ve been terrified ever since. But now? I’m not just scared-I’m empowered.
I quit smoking last week. Started walking daily. Got my BP checked. It’s 124/78. I’m not waiting for a catastrophe. I’m taking back my health. And yes, I’m doing annual MRIs. But I’m not losing sleep anymore. Thank you for giving me hope, not fear.
PS: I’m telling all my friends. This needs to be viral.
eric fert
Let’s be real. All these ‘risk scores’ are just fancy math to justify expensive procedures. You know who benefits? The hospitals. The device companies. The neurosurgeons who get paid per clip or coil.
Meanwhile, the patient gets a lifetime of scans, meds, anxiety, and maybe a scar they didn’t need. And let’s not forget the 15% of coiled patients who come back for another go-round. It’s a revolving door.
And don’t get me started on flow diverters-$50,000 stents that require you to take blood thinners for a year. For a condition that might never kill you. Are we treating brains or balance sheets?
Observation isn’t passive. It’s the most radical choice in modern medicine.
And yes, I know I sound like a conspiracy theorist. But I’ve seen too many people get ‘saved’ by surgery… only to die five years later from a stroke they got because of the antiplatelets.
Napoleon Huere
There’s a quiet tragedy in modern medicine: we treat aneurysms like enemies to be destroyed, not parts of a living system to be understood.
The body doesn’t make weak spots by accident. There’s always a story-genetics, stress, inflammation, even emotional tension. We fix the bubble, but never ask why the wall gave way.
Maybe the real cure isn’t in titanium clips or platinum coils… but in learning how to live with less pressure. Not just in the arteries. In the soul.
What if the best treatment for an aneurysm isn’t surgery… but stillness?
Aishah Bango
People need to stop treating their bodies like they’re disposable. Smoking? Drinking? Ignoring BP? That’s not a lifestyle-it’s self-neglect dressed up as freedom.
If you’re going to destroy your health, don’t act surprised when it breaks. You didn’t get an aneurysm because of bad luck. You got it because you made choices. And now you want a magic fix?
Stop looking for tech solutions to moral failures.
SWAPNIL SIDAM
I’m from India. We don’t have access to all this fancy tech. My cousin had an aneurysm. They didn’t even have MRA. Just a CT. They watched. He lived. He quit smoking. He walks every morning. No surgery.
Maybe the best treatment is just… care. Not cost.
Geoff Miskinis
One must question the statistical validity of these PHASES scores when derived from predominantly Western cohorts. The cultural and genetic heterogeneity of South Asian populations-particularly regarding hypertension thresholds and aneurysm morphology-is grossly underrepresented in the literature.
Applying these risk algorithms to non-European populations is not merely suboptimal-it is epistemologically colonial. One wonders if the ‘3.2% global prevalence’ is even meaningful when 70% of the world’s population is excluded from the dataset.
And yet, here we are. Treated as data points, not patients.
Betty Bomber
My dad had a coiled aneurysm. He’s fine. But he still checks his BP every morning. Still doesn’t drink. Still walks. No drama. No fear. Just… habits.
This post? Perfect. No fluff. Just facts. Thanks.
Mohammed Rizvi
Smoking’s the real villain here. I used to think ‘one cigarette’ didn’t matter. Then I read that 47% extra risk on top of 3.1x… that’s not a number. That’s a death sentence written in nicotine.
I quit last year. My wife says I’m more patient now. Maybe it’s the lack of carbon monoxide. Or maybe it’s knowing I didn’t gamble with my brain.
Best decision I ever made.
Curtis Younker
Hey everyone-just wanted to say this post saved my life. Seriously.
I’m 41, had a 5mm aneurysm found last year. I was ready to sign up for surgery. Then I saw the PHASES score breakdown. My score was 4. Low risk. No smoking. BP normal. I chose observation.
Now I’m doing yoga, eating clean, and getting scans every 12 months. I’m not just surviving-I’m thriving. And I’m telling everyone I know. If you’ve got an aneurysm? Don’t panic. Do the math. Ask the right questions. And take back your power.
You’ve got this. 💪❤️