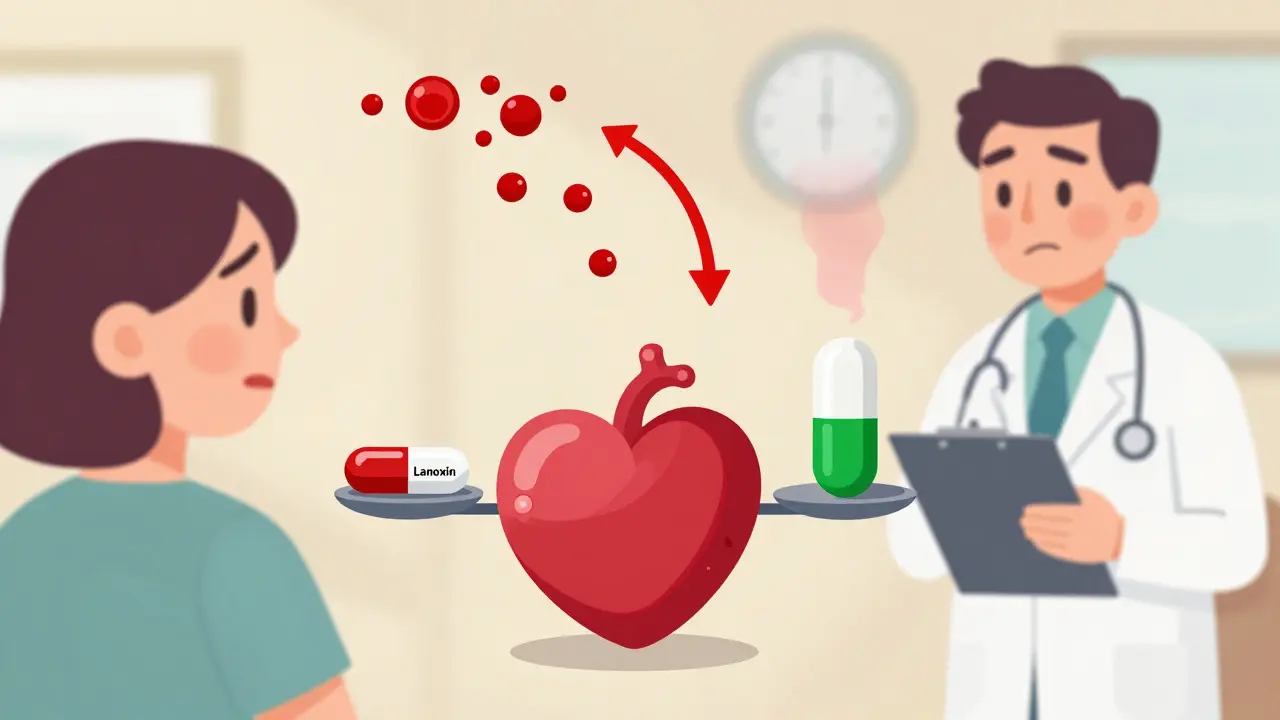
When you take digoxin, even a tiny change in how your body absorbs it can mean the difference between healing and hospitalization. This isn’t just another pill. Digoxin is a narrow therapeutic index drug - meaning the gap between a helpful dose and a dangerous one is razor-thin. For heart failure and atrial fibrillation, the safe range is 0.5 to 2.0 ng/mL. Go below 0.5, and your heart may not get the support it needs. Rise above 2.0, and you risk deadly arrhythmias, nausea, confusion, or even sudden death.
Why Generic Digoxin Isn’t Like Other Generics
Most generic drugs are safe swaps. Take ibuprofen or metformin - the active ingredient is the same, and your body treats it the same way. But digoxin? It’s different. The FDA treats it like a new drug, not just a copy. Why? Because small differences in how it’s made - the fillers, the coating, the manufacturing process - can change how much of the drug actually gets into your bloodstream. In 2002, the FDA set a strict rule: any generic digoxin must prove it delivers the same amount of medicine as the brand-name Lanoxin. The standard? The 90% confidence interval for absorption (measured by AUC and Cmax) must fall between 80% and 125% of Lanoxin. That sounds tight enough, right? But here’s the catch: that rule applies to the average across a group of people. One person might absorb only 45% of the dose from a generic. Another might absorb 110%. The average could still pass the test - even if one patient is getting too little or too much.What Happens When You Switch Generics
Most patients never think twice about switching from one generic to another. Pharmacists do it all the time - cheaper stock, better insurance coverage, supply issues. But with digoxin, that switch can be risky. A 2023 review in US Pharmacist found that while each generic digoxin product may be bioequivalent to Lanoxin, there are no studies proving they’re bioequivalent to each other. That means if you’ve been stable on Generic A for months, and your pharmacy switches you to Generic B without telling you, your blood levels could jump or drop by 25% or more. That’s enough to cause toxicity or make your heart condition worse. Real cases back this up. Patients on stable doses of digoxin have been admitted to the ER after a generic switch - not because they missed a pill, but because the new version absorbed differently. Elderly patients are especially vulnerable. Their kidneys clear digoxin slower. Their bodies are less forgiving. One small change in absorption can pile up over days, since digoxin has a half-life of 36 hours. That means it sticks around. If you start absorbing more, it doesn’t just go away when you stop taking it.Formulation Matters: Tablets vs. Elixir
Not all digoxin is the same - even within the same brand. The tablet form is absorbed at about 60-80% efficiency. But the liquid version? It’s absorbed better: 70 to 85% of the dose gets into your blood. That’s a big deal if you’re switching from a tablet to an elixir - or vice versa - without adjusting your dose. Some patients, especially those with swallowing issues or poor gut absorption, are prescribed the liquid form. But if you’re suddenly switched back to tablets without a dose change, your digoxin levels could fall below therapeutic levels. Symptoms like fatigue, dizziness, or worsening shortness of breath might show up - and get mistaken for heart failure getting worse, not because the drug isn’t working, but because your body isn’t absorbing it the same way.
Monitoring: It’s Not Optional - It’s Essential
If you’re on digoxin, regular blood tests aren’t a suggestion. They’re a necessity. The American College of Clinical Pharmacy recommends measuring serum digoxin levels before your next dose - that’s the trough level. That’s when the drug is at its lowest, and the most accurate reflection of your steady-state concentration. Here’s what you need to know:- Target range: 0.5-2.0 ng/mL
- Optimal range for heart failure: 0.5-0.9 ng/mL (lower is safer and just as effective)
- Check levels 4-7 days after starting digoxin or changing the dose
- Check levels again 3-5 days after switching manufacturers or formulations
- Check levels whenever your kidney function changes - or if you start or stop another medication
What Patients and Providers Should Do
If you’re on digoxin, here’s what you need to do:- Know which brand or generic you’re taking. Write it down. Keep the bottle.
- Ask your pharmacist: “Is this the same digoxin I’ve been taking?” Don’t assume.
- If you’re switched to a new generic, watch for symptoms: nausea, vomiting, blurred vision (yellow or green halos), irregular heartbeat, extreme fatigue.
- Request a digoxin blood test 3-5 days after any change - even if you feel fine.
- Ask your doctor if you’re on the lowest effective dose. Many patients are on too much.
- Avoid switching digoxin products unless absolutely necessary.
- If you must switch, document the change and schedule a follow-up blood test.
- Consider using the same generic consistently - even if it’s slightly more expensive. The cost of a hospitalization for toxicity far outweighs the drug cost.
- Don’t rely on patient reports alone. Symptoms of digoxin toxicity are vague and easily missed.
The Bigger Picture: NTI Drugs Need Special Care
Digoxin isn’t alone. Warfarin, lithium, phenytoin, cyclosporine, and tacrolimus are all narrow therapeutic index drugs. They all need the same level of attention. But digoxin is one of the most commonly prescribed NTI drugs - especially in older adults. And yet, it’s often treated like an afterthought. The American Heart Association and American College of Cardiology both say: use the same manufacturer’s product when possible. That’s not a suggestion. It’s a safety rule. Generic drugs saved billions in healthcare costs. But with NTI drugs, savings shouldn’t come at the cost of safety. The FDA’s rules are strong - but they’re based on population averages. Real people don’t live in averages. They live in their own bodies. And for someone on digoxin, their body’s response is the only thing that matters.Bottom Line: Don’t Guess. Test.
Digoxin generics are not dangerous because they’re generic. They’re dangerous because we treat them like they’re interchangeable - and they’re not. The science says they’re bioequivalent on paper. But in real life, with real patients, the differences matter. The fix isn’t to stop using generics. It’s to treat digoxin like the high-risk drug it is. Know what you’re taking. Monitor levels. Don’t switch without checking. And if you’re on digoxin - whether it’s brand or generic - make sure your doctor knows. And make sure they’re checking your blood.Your heart can’t afford to guess.







Isabella Reid
My grandma’s on digoxin and her pharmacist switched her to a cheaper generic last month. She started feeling dizzy and nauseous - we thought it was just aging, but turns out her levels spiked. Got her tested and bam, 2.4 ng/mL. Scary stuff. Now we insist on the same brand every time. Don’t let savings kill you.
Also, why do pharmacists never tell you when they switch? Like, a simple ‘hey, this is a different maker’ would save lives.
swarnima singh
so like… if your body absorbs less, does that mean the pill is just… poof? gone? like magic? or is it just sitting in your gut being passive aggressive? 😭
Jody Fahrenkrug
I work in a nursing home and we’ve had two patients admitted for digoxin toxicity after a generic switch. One was 89, didn’t even notice she felt ‘off’ until she started seeing yellow halos around the lights. Her daughter cried when she found out it was just a pharmacy change. No one warned them. This needs to be on every script label.
Also - liquid vs tablet? We had a guy on elixir for years, got switched to tablet without dose adjustment. His levels dropped 40%. He thought he was just ‘getting weaker.’
Kasey Summerer
So let me get this straight - we’re saying a pill that costs $3 can kill you, but the $15 version is ‘safer’? 😂
Pharma companies are laughing all the way to the bank while grandmas hallucinate yellow halos. Classic capitalism. 🤡
Allen Davidson
My dad’s been on digoxin for 12 years. We switched generics twice because of insurance changes. He never had symptoms, but we got his levels checked both times anyway. First time: fine. Second time: dropped to 0.42. We switched back immediately. No drama. Just blood tests.
Don’t wait for symptoms. Test. It takes 10 minutes and costs $40. Way cheaper than an ER visit.
Also - if your doctor won’t order the test, find a new doctor. This isn’t optional.
john Mccoskey
Let’s be brutally honest here - the entire generic drug system is a facade for cost-cutting at the expense of patient safety. The FDA’s 80-125% bioequivalence range is a joke when you’re dealing with a drug where 0.1 ng/mL can mean the difference between life and death. This isn’t about ‘individual variability’ - it’s about regulatory capture. The pharmaceutical lobby ensures that the system remains broken because it’s profitable. And now we’re blaming patients for not monitoring their levels? No. We’re blaming a system that incentivizes cutting corners on life-saving medication. Digoxin is the canary in the coal mine. Warfarin, lithium, phenytoin - they’re next. And nobody’s talking about it. Because nobody wants to admit that the entire ‘generic equals safe’ narrative is a lie sold to the public by people who profit from it. Wake up.
And yes, I’ve seen the charts. The data is there. The studies exist. The deaths are documented. But the FDA won’t change the rules because it’s too expensive to reclassify every NTI drug as ‘non-interchangeable.’ So we keep pretending it’s fine. It’s not.
vivek kumar
India’s generic market is massive, but digoxin is one of the few drugs we actually regulate tightly. Still, many rural pharmacies don’t track batches. I had a patient switch from one Indian generic to another - no one knew the manufacturer changed. His creatinine was high, his levels were 2.8. He thought he was ‘getting better’ because he stopped feeling tired - turns out, he was in early toxicity. We had to dialyze him.
Bottom line: even in countries with cheap generics, you can’t skip monitoring. Period.
Henry Ip
My aunt switched from brand to generic and felt fine for weeks. Then one morning she couldn’t stand up. Took her to the ER - digoxin level was 3.1. They said it was likely the new generic. She’s fine now but scared to even touch meds. I asked her pharmacist why no one warned her. He said ‘we assumed the doctor knew.’
Doctors don’t know. Pharmacists don’t tell. Patients don’t ask. That’s the problem.
Just test. It’s easy.
waneta rozwan
I’m a nurse and I’ve seen this too many times. One woman was on digoxin for 15 years. Got switched to a new generic. Two weeks later, she was in cardiac arrest. They revived her. She didn’t even know she’d been switched. Her daughter found the pill bottle and noticed the name was different. She called me crying. ‘Why didn’t anyone tell us?’
Because no one cares. Until someone dies.
And now she’s terrified to take any pill. Can you blame her?
Chelsea Harton
just test your levels. that’s it. no drama. no fear. just a blood draw. you’re already taking the pill. why not check if it’s working?
brooke wright
wait so if you’re on liquid digoxin and switch to tablet without adjusting - you’re basically giving yourself a 20% dose reduction? that’s wild. my uncle was on liquid for years because he couldn’t swallow pills. then they switched him because ‘it’s cheaper’ and he started falling down. we thought he was having mini strokes. turns out his heart was just… not getting enough. they didn’t even think to check digoxin levels. why? because they think it’s just ‘a heart pill.’ it’s not. it’s a landmine.
also why is no one talking about how often pharmacists don’t even know this? i asked mine and she said ‘oh yeah, i heard something about that once.’
Nick Cole
My mom’s on digoxin. I printed out the FDA guidelines and gave them to her pharmacist. She didn’t know any of this either. We now have a note on her file: ‘DO NOT SWITCH DIGOXIN MANUFACTURER WITHOUT CONSULTATION.’
It’s not hard. It’s just not common.
Do the thing. Save a life.
swarnima singh
you know what’s worse? when your doctor says ‘it’s all the same’ and you’re too scared to argue. i used to believe that. until i almost died. now i carry my pill bottle like a trophy.