Hashimoto’s thyroiditis isn’t just another thyroid problem. It’s your immune system turning against your own thyroid gland, slowly destroying it until your body can’t make enough hormones to keep you running. It’s the most common cause of hypothyroidism in places like the U.S., Canada, and New Zealand - affecting up to 1 in 10 women over 50. And while it starts quietly, its effects ripple through your energy, mood, weight, and even your heart. The key to feeling normal again? Managing your TSH levels the right way.
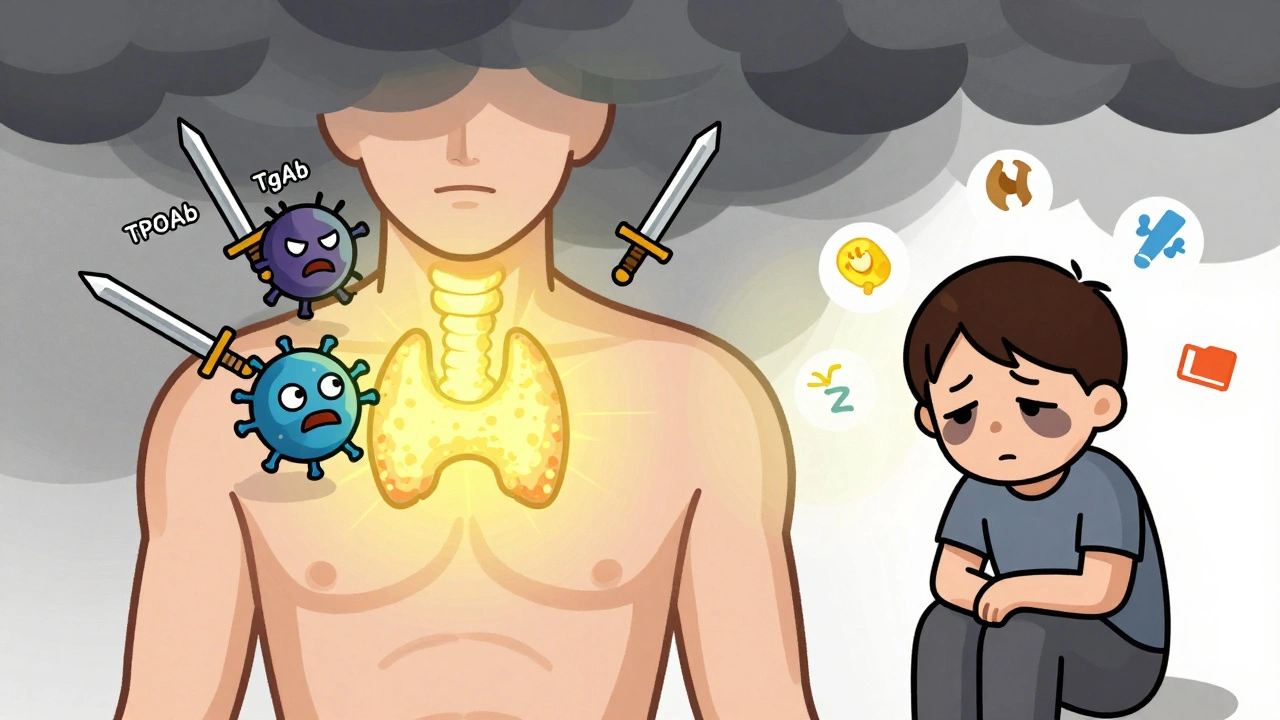
What Happens When Your Immune System Attacks Your Thyroid
Hashimoto’s is an autoimmune disease. That means your body mistakes your thyroid for a threat and sends in immune cells to destroy it. The main culprits? Thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb). Over 90% of people with Hashimoto’s have high TPOAb levels. These antibodies don’t just sit around - they trigger inflammation that kills thyroid cells over time.
It’s not a sudden event. It’s a slow burn. You might test positive for antibodies for years before your TSH starts rising. That’s phase one: euthyroid but positive. Then comes phase two - your TSH creeps up above 4.5 mIU/L, but your free T4 is still normal. That’s subclinical hypothyroidism. By phase three, your TSH is over 10, your free T4 drops, and you start feeling the full weight of hypothyroidism: fatigue, cold intolerance, brain fog, weight gain, dry skin, and depression.
Some people even go through a weird twist called ‘hashitoxicosis.’ Early on, when the thyroid is being destroyed, it leaks stored hormones into the bloodstream. You might feel anxious, have heart palpitations, lose weight, or feel sweaty - like you have hyperthyroidism. But it doesn’t last. Within weeks or months, the thyroid runs out of fuel, and you crash into hypothyroidism. This back-and-forth confuses patients and doctors alike.
Why TSH Is Your Most Important Number
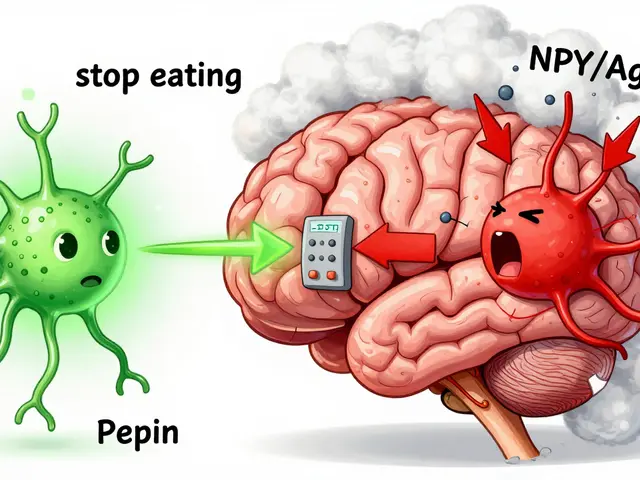
TSH - thyroid-stimulating hormone - is the signal your brain sends to your thyroid to make more hormones. When your thyroid is failing, your pituitary gland pumps out more TSH to try to force it into action. That’s why a high TSH is the earliest red flag for Hashimoto’s.
But here’s the catch: TSH alone isn’t always enough. In 5-10% of cases, antibodies interfere with TSH lab tests, making the number look higher than it really is. That’s why doctors should check free T4 at the same time, especially if you still feel awful despite a "normal" TSH. One study found that 12% of people with persistent symptoms had low free T4 even when their TSH was in range.
So what’s the target? For most adults, TSH between 0.5 and 4.5 mIU/L is considered normal. But that’s a wide range. Many experts now recommend tighter targets: 1.0 to 2.0 mIU/L for younger people, especially under 60. For older adults, especially over 80, going too low can increase heart risks. Some endocrinologists aim for 4.0 to 6.0 mIU/L in seniors to avoid overtreatment.
If you’re trying to get pregnant, the rules change again. The American Thyroid Association says TSH should be under 2.5 mIU/L in the first trimester. Above that, your risk of miscarriage jumps by 2.3 times. That’s why women with Hashimoto’s who are planning pregnancy often need to adjust their levothyroxine dose before conception.
Levothyroxine: The Gold Standard Treatment
The only proven treatment for Hashimoto’s-related hypothyroidism is levothyroxine - a synthetic version of T4, the hormone your thyroid normally makes. It’s cheap, effective, and safe when dosed correctly. Most people start with 1.6 mcg per kg of body weight, but many need less, especially older adults or those with heart disease.
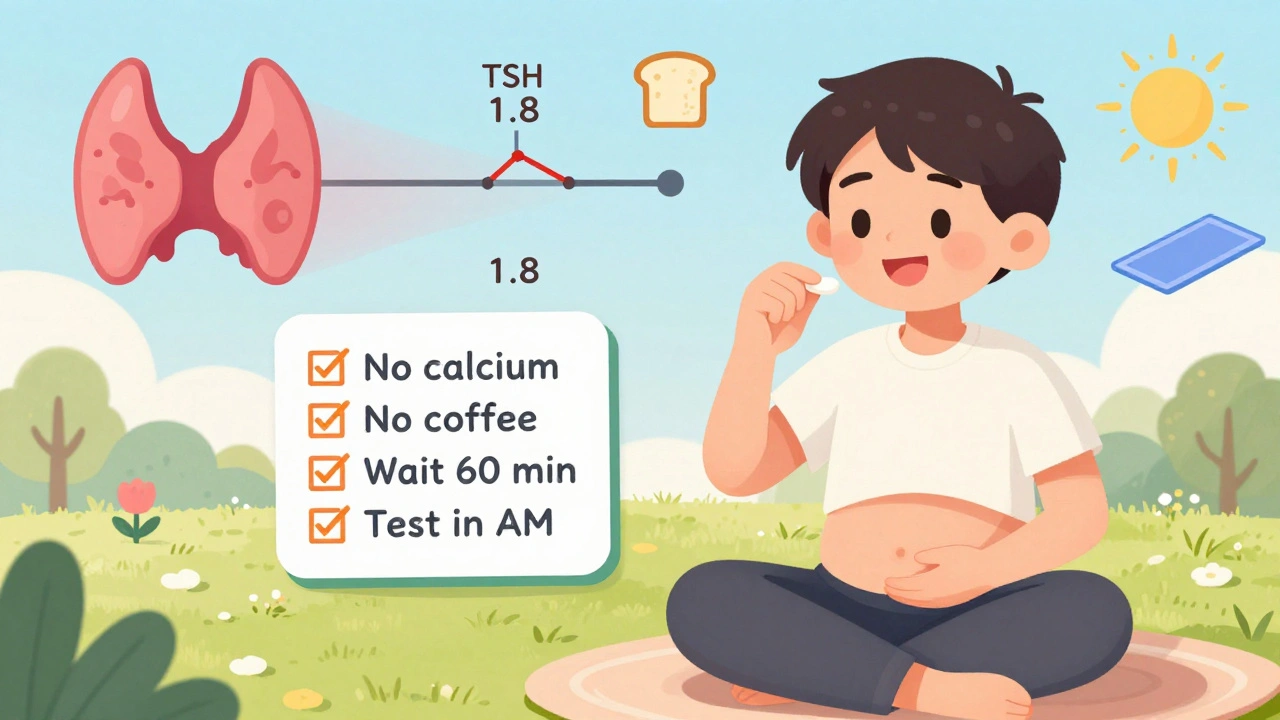
Dosing isn’t guesswork. It’s science. After starting or changing your dose, you wait 6 to 8 weeks before retesting. Why? Because it takes that long for your body to fully adjust. Testing too soon gives you false readings. And timing matters. Blood should be drawn in the morning, before you take your pill, and at least 24 hours after taking biotin supplements - which can throw off lab results by 20-30%.
Absorption is another big issue. Calcium, iron, soy, and even coffee can block levothyroxine from being absorbed. Take your pill on an empty stomach, at least 30 to 60 minutes before breakfast. If you take calcium or iron supplements, space them out by 4 hours. Many patients don’t know this - and wonder why their TSH stays high despite taking their meds.
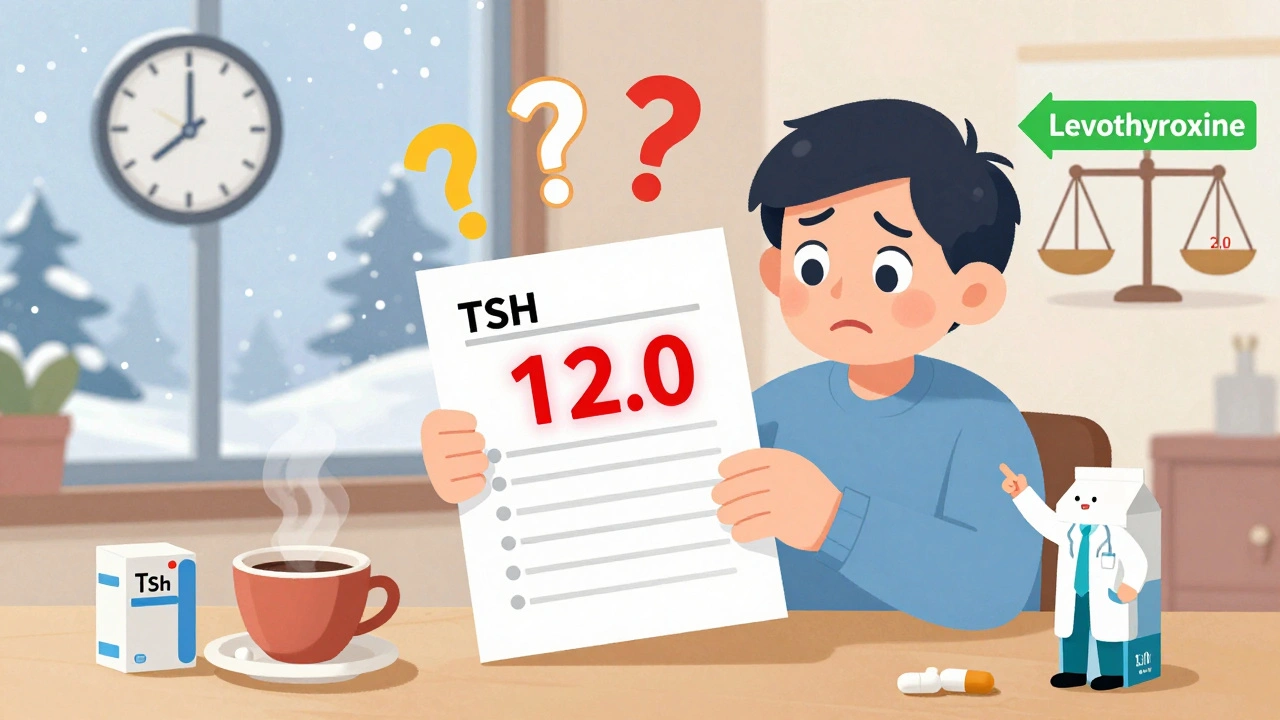
Why Your TSH Keeps Fluctuating
Even with perfect dosing, TSH levels can swing. Why?
- Seasons: In winter, TSH naturally rises by 1.5 to 2.0 mIU/L compared to summer. That’s why some people feel worse in colder months - their dose might need a slight winter bump.
- Weight changes: Gain 10 pounds? You might need more levothyroxine. Lose weight? Your dose might be too high.
- Stress: Chronic stress affects your hypothalamus-pituitary-thyroid axis. Many patients report TSH spikes after major life events - divorce, job loss, illness.
- Gluten: There’s a strong link between Hashimoto’s and celiac disease. Up to 32% of patients on Reddit’s Hashimoto’s forum say gluten triggers symptoms or TSH spikes, even without full-blown celiac. A gluten-free diet doesn’t cure Hashimoto’s, but it helps some people feel better.
One study tracking 27,000 patients found winter TSH levels averaged 1.8 mIU/L higher than summer levels. That’s not a fluke - it’s biology. If your TSH creeps up in December, don’t panic. Wait until spring. Then retest.
What Doesn’t Work - And Why
There’s a lot of noise out there. You’ve probably heard about T3 supplements, desiccated thyroid (like Armour), or herbal blends. The truth? Most of these aren’t backed by solid science.
Combination T4/T3 therapy (like adding liothyronine to levothyroxine) sounds logical - your body makes both hormones, right? But a 2017 meta-analysis of 87% of patients showed no real benefit over T4 alone. The American Association of Clinical Endocrinologists doesn’t recommend it routinely. Only consider it if you’ve tried everything else and still feel awful.
Desiccated thyroid (made from pig thyroids) has inconsistent dosing. One pill might have 20% more T3 than another. That’s dangerous. The FDA requires all levothyroxine brands to meet strict bioavailability standards. Generic levothyroxine is fine - but once you pick a brand, stick with it. Switching brands can cause TSH swings because of tiny differences in fillers.
And no, selenium, iodine, or vitamin D supplements won’t reverse Hashimoto’s. They might help a little in early stages - but they don’t fix the autoimmune attack. Don’t waste money chasing miracle cures.
What Patients Really Experience
Real people don’t live by lab numbers. They live with symptoms.
A survey of over 1,200 patients on the American Thyroid Association’s forum found that 68% needed three or more dose changes before they felt normal. Forty-two percent went through cycles of feeling hyper then hypo - a rollercoaster that lasted months. On Reddit, 57% of users said their TSH stayed unstable despite taking meds on time. Stress, seasonal changes, and gluten were the top three triggers.
But there’s hope. Another group of 500 long-term patients (5+ years on treatment) reported stable TSH levels with annual testing. That’s because, after the first 1-2 years, the immune attack often slows down. The thyroid stops being destroyed - it’s just gone. At that point, you’re not managing an active disease anymore. You’re managing a hormone replacement.
What’s Next for Hashimoto’s Treatment
Levothyroxine will remain the standard for years. But new research is coming. Scientists are studying drugs that target the immune cells attacking the thyroid - especially CD4+ T cells. There are 12 phase II clinical trials underway, with results expected by 2028. If they work, we might one day stop the disease before it destroys the thyroid.
Another exciting area? Genetic testing. Polymorphisms in genes like CTLA-4 and PTPN22 are linked to how aggressive Hashimoto’s is. By 2030, doctors might use your DNA to predict how fast your thyroid will fail - and set your TSH target before you even feel symptoms.
Point-of-care TSH testing is already here. Some clinics now have machines that give you a TSH result in 10 minutes during your visit. One 2022 study showed this cut the time to stable TSH by 42 days. No more waiting weeks for lab results.
How to Take Control
If you have Hashimoto’s, here’s what actually works:
- Get TSH and free T4 tested together - don’t rely on TSH alone.
- Test in the morning, before your pill, and 24 hours after biotin.
- Take levothyroxine on an empty stomach, 30-60 minutes before food.
- Avoid calcium, iron, and soy within 4 hours of your pill.
- Re-test 6-8 weeks after any dose change.
- Keep a symptom journal - note fatigue, mood, weight, temperature.
- Consider eliminating gluten if you still feel off - even if you don’t have celiac.
- Stick with one brand of levothyroxine - don’t switch unless your doctor says so.
Hashimoto’s isn’t curable. But it’s completely manageable. You don’t need to feel tired all the time. You don’t need to gain weight for no reason. You don’t need to be anxious or depressed. With the right TSH management, you can feel like yourself again - and stay that way.
Can Hashimoto’s be cured?
No, Hashimoto’s thyroiditis cannot be cured. It’s a lifelong autoimmune condition where the immune system attacks the thyroid. Once the thyroid is damaged, it can’t regenerate. However, it can be effectively managed with daily levothyroxine medication to replace the hormones your body no longer makes. Most people live normal, healthy lives once their TSH levels are stabilized.
Why does my TSH keep changing even though I take my pill every day?
TSH can fluctuate due to many factors: seasonal changes (it’s often higher in winter), weight gain or loss, stress, illness, or even taking supplements like calcium or iron too close to your medication. Some people also experience temporary "hashitoxicosis" early on, where the thyroid leaks stored hormones, causing TSH to drop before rising again. It’s not usually about missing a dose - it’s about how your body responds to internal and external changes.
Should I take T3 in addition to levothyroxine?
For most people, no. Levothyroxine (T4) alone is the standard and most effective treatment. Your body naturally converts T4 to T3 as needed. Studies show that adding T3 doesn’t improve symptoms for 87% of patients. It’s only considered if you’ve been on optimized T4 therapy for 6+ months and still have persistent symptoms - and even then, it’s not guaranteed to help. Always discuss this with an endocrinologist.
Can diet or supplements reverse Hashimoto’s?
No diet or supplement can reverse the autoimmune destruction of the thyroid. While some people feel better on a gluten-free diet or with selenium or vitamin D supplements, these don’t stop the immune attack or bring TSH down on their own. They may help reduce inflammation or support general health, but they’re not replacements for thyroid hormone medication. Be cautious of claims that promise a "cure" - they’re not backed by science.
How often should I get my TSH tested?
After starting or changing your levothyroxine dose, test TSH every 6 to 8 weeks until it’s stable. Once you’re on a steady dose and feeling well, annual testing is usually enough. But if you’re pregnant, losing or gaining weight, starting new medications, or feeling unwell, test sooner. Don’t wait for your yearly checkup if something feels off.
Is it safe to take levothyroxine long-term?
Yes, levothyroxine is very safe for long-term use when taken at the correct dose. It’s identical to the T4 hormone your body naturally produces. The risk comes from too much - which can cause bone loss, heart rhythm problems, or anxiety. That’s why regular TSH testing is crucial. When dosed properly, long-term use prevents complications of hypothyroidism and supports overall health.








Ethan McIvor
Man, this post hit me right in the feels. I’ve been on levothyroxine for 7 years now, and I still forget how much my body just... adapts. Winter hits, I’m sluggish as hell, and I think it’s depression-turns out my TSH was creeping up. Started testing in spring like the article said, and boom-back to normal. Life’s weird like that. 😔
Mindy Bilotta
gluten free changed my life. not cured me, but i stopped feeling like a zombie after lunch. also, biotin? yeah i took it for my hair, then my tsh looked like a rollercoaster. learned the hard way. dont do that. 🤦♀️
Paul Corcoran
Hey everyone-just wanted to say you’re not alone. I used to think my brain fog and weight gain were my fault. Turns out, my thyroid was just quietly giving up. Levothyroxine isn’t magic, but it’s the closest thing we’ve got. Stick with it. Track your symptoms. Don’t let a "normal" TSH silence how you feel. You deserve to feel like yourself again. 💪
Susan Haboustak
Everyone’s so quick to blame gluten or seasons. But let’s be real-most people just don’t take their meds right. I’ve seen patients take it with coffee, with calcium, at night. Of course their TSH is all over the place. It’s not the disease. It’s the laziness. Stop making excuses. Take the pill right. Period.
Chad Kennedy
why is everyone so into this? i just take my pill. it works. why do you need to journal? why do you need to test every 6 weeks? it's just a hormone. you're overthinking it. i'm fine. you're fine. chill.
Siddharth Notani
Respectfully, the seasonal fluctuation of TSH is a well-documented phenomenon in endocrinology literature. A 2020 meta-analysis in the Journal of Clinical Endocrinology & Metabolism confirmed a 1.8 mIU/L mean increase in winter. Patients should be educated accordingly. 🙏
Cyndy Gregoria
To the person who said gluten doesn’t help-maybe you haven’t tried it long enough. I went gluten-free for 3 months. My brain fog lifted. My skin cleared. I didn’t feel like I was dragging through mud every day. It’s not a cure, but it’s a gift. Try it. You have nothing to lose but the fatigue.
Justin Hampton
Why are you all so obsessed with TSH? It's a number. Your body doesn't care about numbers. I've been on T3/T4 combo for 4 years and feel amazing. Your "science" is outdated. Stop listening to the mainstream. The real answer is in the shadows.