Deep Vein Thrombosis (DVT): Quick Facts You Need
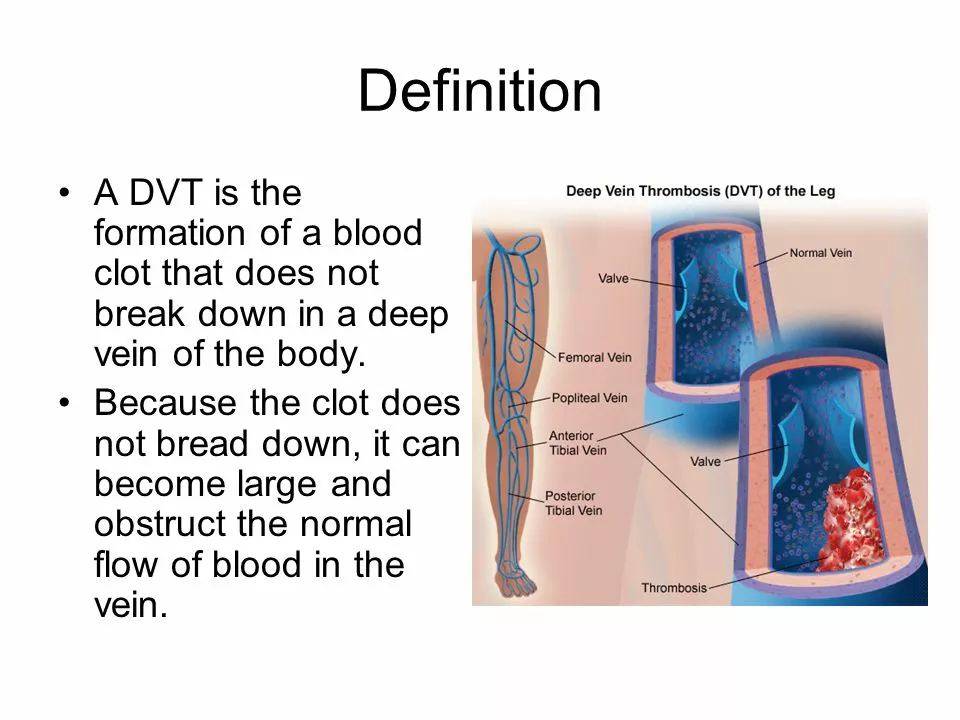
If you’ve ever heard of a blood clot in your leg and felt uneasy, you’re probably thinking about deep vein thrombosis. DVT happens when a clot forms in the deep veins, usually in the thigh or calf. The clot can block blood flow, cause swelling, and in worst cases travel to the lungs – that’s a pulmonary embolism, a medical emergency.
Most people don’t realize they’re at risk until symptoms pop up. That’s why it helps to know the warning signs early and understand what puts you on the DVT radar.
What Is Deep Vein Thrombosis?
DVT is a clot that builds up in veins deep inside your body, not the ones you can see under your skin. The clot forms when blood thickens, the vein wall gets damaged, or blood flow slows down – what doctors call Virchow’s triad.
Common triggers include long flights, sitting for hours at a desk, recent surgery, or injuries to the leg. Even genetics play a role; some families have clotting disorders that make clots more likely.
How to Spot a Blood Clot
The most common sign is swelling in one leg, often accompanied by warmth and redness. You might also feel a cramp‑like pain that gets worse when you stand or walk. If the skin looks shiny or feels tight, those are red flags too.
Because symptoms can look like a muscle strain, never ignore sudden leg discomfort after a long trip or a period of inactivity. If you notice any of these signs, call your doctor right away – early treatment can stop a clot from growing or moving.Treatment usually starts with blood‑thinning medication, called anticoagulants. These drugs keep the clot from getting bigger and reduce the chance of new clots forming. In some cases, doctors may use a filter placed in the large vein that leads to the heart, especially if you can’t take anticoagulants.
Recovery also means moving more. Simple leg exercises, walking, or using compression stockings can boost circulation and lower future risk. If you’re planning a long trip, stand up every hour, stretch, and stay hydrated – these small steps make a big difference.
Knowing your personal risk factors helps you act fast. Talk to your healthcare provider about family history, any recent surgeries, or medications that might affect clotting. They can suggest personalized prevention plans, like low‑dose aspirin or tailored compression gear.
Bottom line: DVT isn’t rare, but it’s manageable when you catch it early and follow treatment advice. Keep an eye on leg swelling, stay active, and don’t hesitate to get medical help if something feels off. Your legs will thank you for the extra care.
Traveling on blood thinners is safe if you follow key steps: take your meds consistently, move often, wear compression stockings, and know the warning signs of blood clots. Learn how to prevent DVT during international trips.
As a blogger, I've recently delved into the role of physical therapy in DVT rehabilitation. I discovered that physical therapy plays a crucial part in helping patients improve their mobility and reduce the risk of complications. By incorporating exercises and manual therapy, therapists can help break down blood clots and enhance blood circulation. Additionally, they provide guidance on compression garments and lifestyle changes to prevent recurrence. Overall, physical therapy offers invaluable support for individuals recovering from DVT, promoting a healthier and more active lifestyle.