Medicare Part D Formulary: What Drugs Are Covered and How to Choose
When you sign up for Medicare Part D formulary, a list of prescription drugs covered by your Medicare drug plan. Also known as a drug list, it tells you exactly which medications your plan will pay for—and which ones won’t. This isn’t just paperwork. It’s the difference between paying $5 or $500 for your diabetes pill, blood pressure med, or arthritis drug.
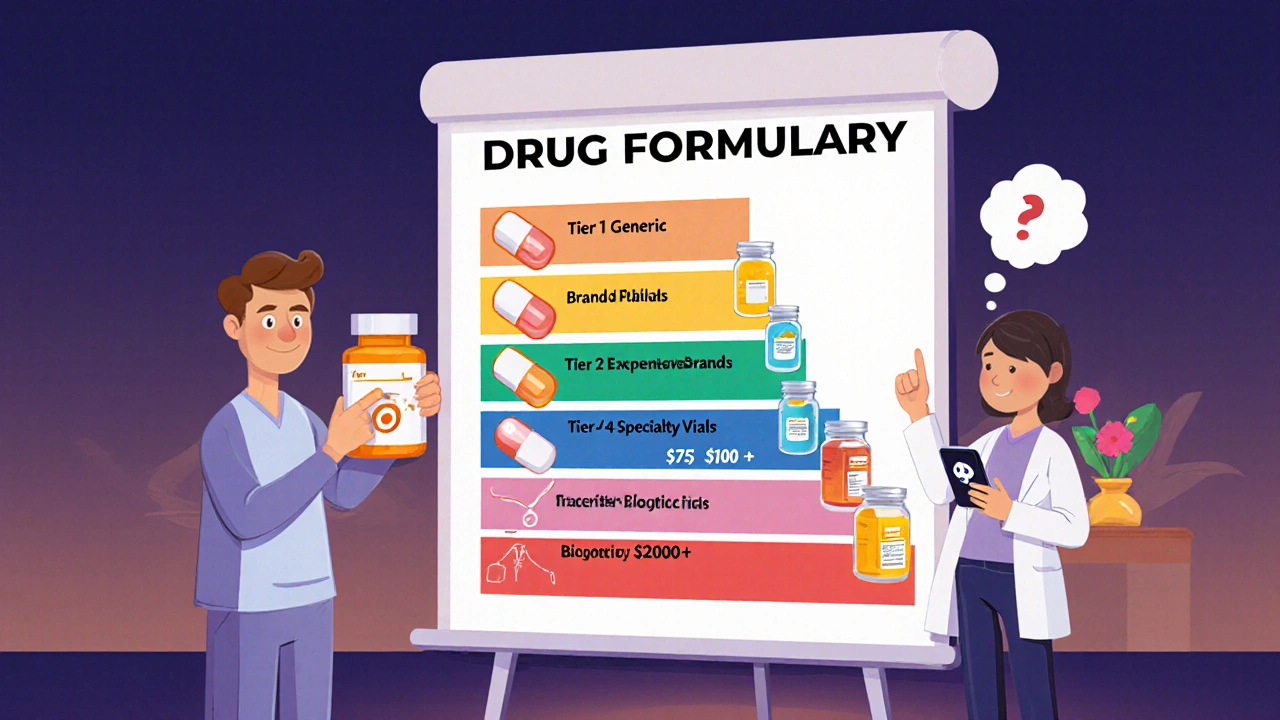
Every Medicare Part D plan has its own formulary, and they’re not all the same. Some cover generic versions only. Others include brand-name drugs but put them in higher cost tiers. The formulary tiers, the cost levels assigned to drugs based on price and preference matter a lot. Tier 1 usually means low-cost generics. Tier 4 or 5? That’s often expensive specialty drugs with high copays. If you take multiple meds, you need to check if your entire list is covered before choosing a plan. A plan that covers your insulin but not your cholesterol drug could cost you more in the long run.
Some plans require prior authorization, a process where your doctor must prove a drug is necessary before the plan pays for it. Others use step therapy, a rule that forces you to try a cheaper drug first before they’ll pay for the one your doctor prescribed. These rules exist to save money—but they can delay your treatment. If your current meds are working, make sure your plan doesn’t force you to switch. You can also find out if your plan has a Medicare Part D alternative, a different plan option with better coverage for your specific drugs. Many people don’t realize they can switch plans during open enrollment or under special circumstances.
Medicare Part D formularies change every year. A drug you got covered last year might be moved to a higher tier—or dropped entirely. That’s why you need to review your plan’s formulary every fall. If you take a drug like SGLT-2 inhibitors for diabetes, or antihistamines for allergies, or even common pain relievers like diclofenac, check if they’re still listed. Missing a change could mean a surprise bill or a gap in treatment. And if you’re on multiple meds, like levothyroxine and calcium supplements, or taking something like azithromycin for an infection, make sure your plan doesn’t block interactions or require extra steps.
Don’t just assume your plan covers what you need. Use the Medicare Plan Finder tool. Call your pharmacy. Ask your doctor to help you match your meds to a formulary. You’re not just choosing a plan—you’re choosing how much you’ll pay out of pocket for the drugs that keep you healthy. The right formulary doesn’t just save money. It keeps your treatment on track.
Below, you’ll find real guides on how to handle drug shortages, spot dangerous interactions, compare inhalers and diabetes meds, and protect yourself from medication errors—all of which tie directly into what your Medicare Part D formulary does or doesn’t cover.
A drug formulary is your insurance plan's list of covered medications. Learn how tiers, exceptions, and new 2025 rules affect your out-of-pocket costs and how to find the best coverage for your prescriptions.