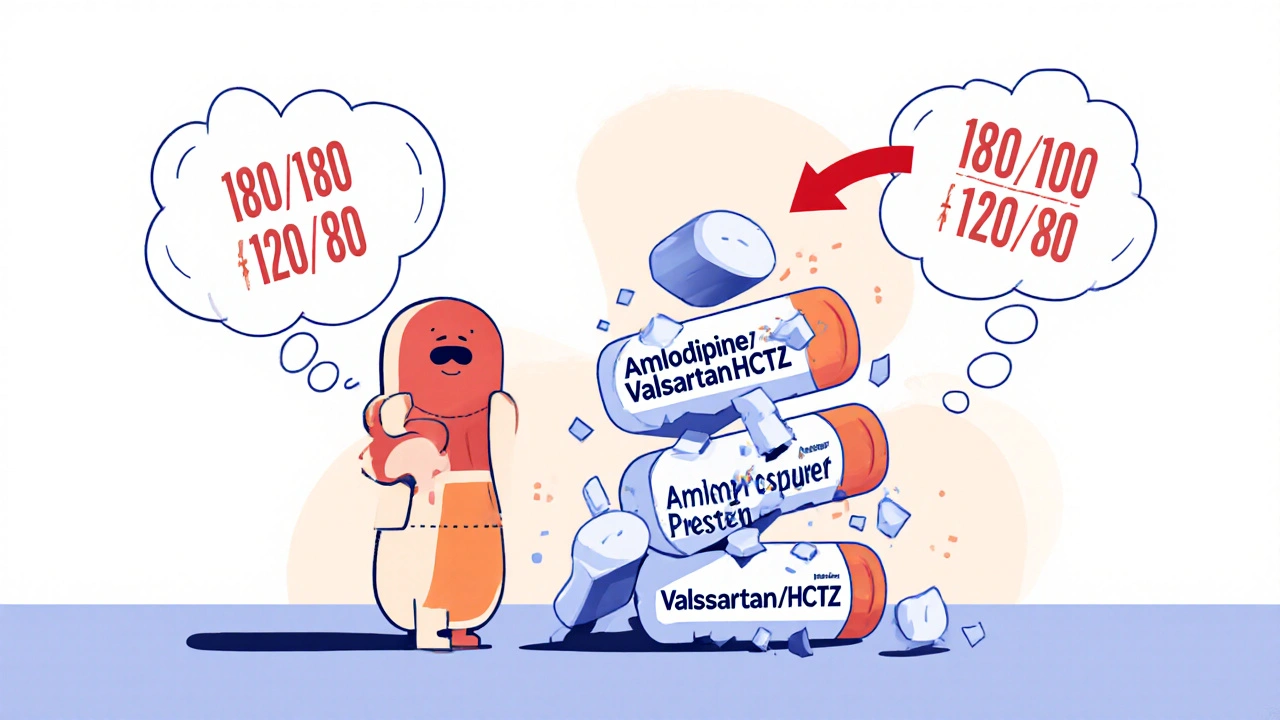
Most people with high blood pressure need more than one pill to get their numbers under control. That’s not a failure - it’s science. About 70 to 80% of patients require two or more medications to hit the target of 130/80 mmHg or lower. But taking three separate pills every day? It’s easy to forget one. That’s where antihypertensive combination generics come in. These are single tablets that pack two or even three blood pressure drugs into one. They’re cheaper than brand names, just as effective, and make life simpler. But here’s the catch: not all combinations are available everywhere, and insurance doesn’t always cover them the way you’d expect.
What Are Antihypertensive Combination Generics?
These are called Single-Pill Combinations (SPCs) or Fixed-Dose Combinations (FDCs). They combine two or three active ingredients from different drug classes into one tablet. Common pairs include:
- Amlodipine + benazepril (a calcium channel blocker + ACE inhibitor)
- Losartan + hydrochlorothiazide (an ARB + diuretic)
- Amlodipine + valsartan (calcium channel blocker + ARB)
Some even have three: amlodipine + valsartan + hydrochlorothiazide. That’s three drugs in one pill. The goal? Reduce pill burden. Studies show people who take one pill instead of three are 15 to 25% more likely to stick with their treatment. That means fewer spikes in blood pressure, fewer ER visits, and less risk of stroke or heart attack.
The FDA requires these generics to match the brand-name versions in how they’re absorbed by the body - within 80% to 125% of the original. That’s not a guess. It’s tested in healthy volunteers with blood samples taken over hours. If it passes, it gets approved. So, no, a generic isn’t weaker. It’s the same medicine, just cheaper.
Which Combinations Are Actually Available?
There are over 30 different antihypertensive combinations on the global market. In the U.S., you can get most of them as generics. Here’s what’s commonly stocked at pharmacies:
- Amlodipine/benazepril - 5/20mg, 10/20mg, 10/40mg
- Losartan/hydrochlorothiazide - 50/12.5mg, 100/12.5mg, 100/25mg
- Valsartan/hydrochlorothiazide - 80/12.5mg, 160/12.5mg, 160/25mg
- Olmesartan/amlodipine - 20/5mg, 40/5mg, 40/10mg
- Trileptal (amlodipine/valsartan/HCTZ) - 5/160/12.5mg, 10/160/12.5mg
Some combinations are harder to find. For example, if you need amlodipine 2.5mg with valsartan 160mg, you’re out of luck. That exact dose doesn’t exist in a single pill. You’d have to take two separate tablets. That’s the biggest limitation of SPCs: you can’t adjust the dose of one drug without switching pills entirely.
Cost: Why Sometimes the Combo Costs More Than Two Separate Pills
This is where things get confusing. A few years ago, combination pills were cheaper than buying the two drugs separately. That’s not always true anymore.
Here’s the reality: if both individual drugs are generic, buying them separately often costs less. For example:
- Generic amlodipine (5mg): $4.50/month
- Generic valsartan (160mg): $7.80/month
- Generic Exforge (amlodipine/valsartan): $18.75/month
That’s $12.30 for two pills vs. $18.75 for one. Same drugs. Higher price for the combo. Why? Because manufacturers still price SPCs like they’re special. Insurance companies know this. Some will only cover the combo if the individual pills are more expensive - which they usually aren’t anymore.
On GoodRx, you can find:
- Losartan/HCTZ (Hyzaar generic): as low as $10.60/month
- Benazepril/HCTZ (Lotensin HCT): $38.05/month
- Amlodipine/benazepril (Lotrel): $17.55/month
But if you check your local pharmacy, you might find the same drugs sold separately for less. Always compare. Use GoodRx, SingleCare, or your pharmacy’s discount program. Don’t assume the combo is cheaper.
Insurance and Coverage: The Hidden Hurdle
One of the most common complaints? Insurance covers the individual pills for $5 each - but charges $45 for the combo. That’s not a mistake. It’s a policy.
Many insurers have tiered formularies. They’ll put the combo on a higher tier because it’s a single product. Even if the cost to the pharmacy is almost the same, the insurer charges more to discourage use - or because the manufacturer hasn’t negotiated a good rebate.
Patients on Reddit and PatientsLikeMe report this constantly:
- "My copay for the combo is $50. I can get the two pills separately for $10 total. Why does this exist?" - HypertensionWarrior87
- "Insurance won’t approve the combo unless I try the individual meds first. Even though I’m on them already." - BPstruggler
Workaround? Ask your doctor to write a letter of medical necessity. Or switch to the separate pills. If you’re stable on the combo and your insurance denies it, ask for a prior authorization. Some plans will approve it if you show you’ve tried the alternatives.
Why Doctors Still Recommend Them - Even When They Cost More
Despite the cost issues, doctors still push SPCs. Why?
The STRIP trial in 2018 showed that 68% of patients on a combination pill hit their blood pressure goal - compared to just 45% on single pills taken one after another. That’s a huge difference. Adherence is the real game-changer. People forget pills. They get confused. A single pill reduces errors. One study found SPC users had 82.3% adherence vs. 67.1% for free combinations. That’s a 28% drop in hospitalizations for uncontrolled hypertension.
For older adults, people with memory issues, or those juggling multiple meds, the combo is a lifeline. It’s not about cost. It’s about survival.
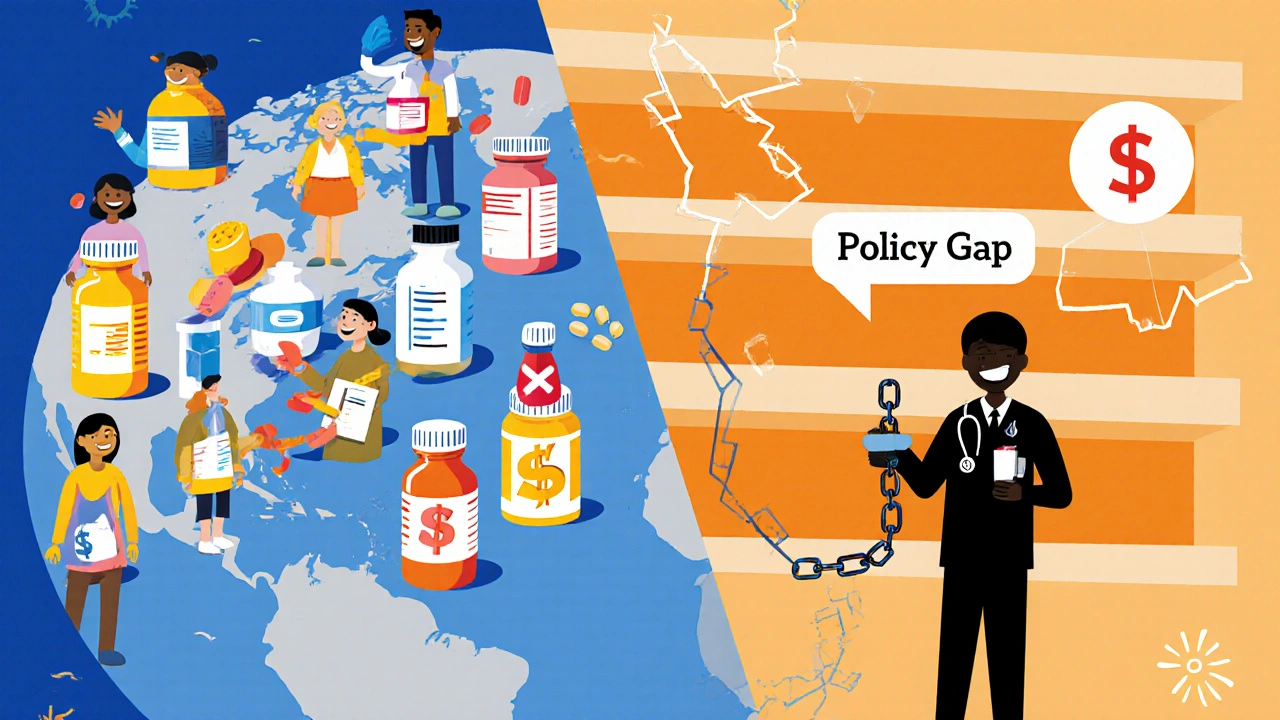
What’s Missing: The Global Gap
Here’s something most people in the U.S. don’t realize: in low-income countries, these pills are often unavailable. The WHO says 95% of hypertension cases need combination therapy. But in 46% of low-income countries, essential medicines - including these combos - are less than 50% available.
Why? Manufacturing, distribution, pricing, and lack of inclusion in national guidelines. Even when the pills exist, clinics don’t stock them. Doctors don’t know how to prescribe them. Patients can’t afford them.
In the U.S., 85% of antihypertensive prescriptions are for generics. In some African and South Asian countries, that number is under 15%. That’s not a technical problem. It’s a policy failure.
How to Get the Right Combination for You
Here’s how to navigate this:
- Ask your doctor: "Is there a generic combo pill that matches my current doses?" Don’t assume they know - many don’t track every available SPC.
- Check your doses: If you’re on amlodipine 2.5mg and valsartan 160mg, you can’t get that in one pill. You’ll need two separate tablets.
- Compare prices: Use GoodRx or your pharmacy’s app. Type in each drug separately and then the combo. Sometimes the combo wins. Often, it doesn’t.
- Call your insurance: Ask: "Is this combination covered? What’s my copay? Is there a preferred generic?" Get it in writing.
- Don’t switch without talking to your doctor: Changing your regimen can cause blood pressure swings. Always consult before making changes.
Future Trends: Triple Combos Are Coming
The FDA is making it easier to approve new generic combinations. In 2023, they released draft guidance to speed up the process. That means more options are coming - especially triple-combination pills.
Studies show triple combos could cut the treatment gap in low-income countries by 35%. For patients here, they mean even fewer pills. Imagine taking one pill instead of three. That’s the future.
But until then, stick with what works. If your current combo is helping you stay under control and you can afford it - keep it. If it’s too expensive or your insurance won’t cover it, ask for the individual generics. You’re not failing. You’re being smart.
Are antihypertensive combination generics as effective as brand names?
Yes. The FDA requires generic combination pills to be bioequivalent to the brand-name version. That means they deliver the same amount of active ingredients into your bloodstream within a narrow, scientifically accepted range (80-125%). Clinical studies show no difference in blood pressure control between generic and branded SPCs. The only difference is cost.
Can I split a combination pill if I need a lower dose?
Some combination pills are scored and can be safely split - like amlodipine/benazepril 10/20mg. But others aren’t designed for splitting. Never split a pill unless your pharmacist confirms it’s safe. Splitting can change how the drug is absorbed, especially if it’s an extended-release formula. Always ask before splitting.
Why won’t my insurance cover my combination pill?
Many insurers prioritize cheaper alternatives. If the two individual generic drugs cost less than the combo, they’ll require you to try them first. This is called "step therapy." You can appeal with a letter from your doctor explaining why the combo is medically necessary - especially if you’ve had trouble adhering to multiple pills.
What if I need a dose that isn’t available in a combo pill?
Many combinations come in fixed doses - like 5mg/20mg or 10mg/40mg. If you need 2.5mg/160mg, that exact combo doesn’t exist. You’ll need to take two separate pills. That’s not a flaw in your treatment - it’s just how the market works. Talk to your doctor about the best way to manage that regimen without losing adherence.
Are there any risks with taking two blood pressure drugs in one pill?
The risks are the same as taking the drugs separately. Combination pills don’t increase side effects - they just make them harder to track. For example, if you get swollen ankles, is it from the amlodipine or the other drug? Your doctor needs to know which component is causing issues. That’s why it’s important to report any new symptoms clearly. If side effects become problematic, switching to individual pills may help identify the culprit.
What to Do Next
Start by listing your current medications. Write down the exact doses. Then check GoodRx or your pharmacy app for prices on both the combo and the individual pills. Talk to your pharmacist - they know what’s in stock and what’s cheapest. If you’re on a combo and it’s working, don’t change it unless cost or coverage forces you to. If you’re on separate pills and struggling to remember them, ask your doctor about switching to a combination. You might be surprised how much simpler your life can become.










amit kuamr
Combination pills are a joke in India. We get the same generics but at 1/10th the price. Here in the US you pay $20 for a pill that costs $2 in Delhi. Pharma companies are laughing all the way to the bank
Scotia Corley
The bioequivalence standards set forth by the FDA are scientifically robust and rigorously enforced. To suggest that generic combination therapies are inferior is to misunderstand the regulatory framework governing pharmaceutical approval. The data are unequivocal.
elizabeth muzichuk
I knew a woman who died from a stroke because her insurance denied her combo pill and made her take three separate ones. She forgot one. They don't care. They just want to save money. This isn't healthcare. It's a profit scheme disguised as medicine.
Debbie Naquin
The pharmacokinetic profile of fixed-dose combinations demonstrates a significant reduction in inter-individual variability in plasma concentration-time curves compared to free combinations. This is due to synchronized absorption kinetics. The adherence advantage isn't behavioral-it's pharmacodynamic. The pill burden reduction alters the entropy of therapeutic compliance. We're not just talking about convenience. We're talking about systemic stability in chronic disease management.
Karandeep Singh
combo pills are overrated. just take two pills. its not that hard. also why do u need 3 drugs anyway??
Mary Ngo
Did you know that the FDA and Big Pharma have a secret handshake? They approve these combos just to keep you dependent. The real cure for hypertension is diet and fasting. But they can't sell that. So they give you pills. And then they charge you $50 for one. It's all a scam. The government knows. They just won't tell you.
James Allen
Look I get it. We're all trying to survive. But come on. We're the most advanced country on earth and we can't get a simple pill combo right? Meanwhile China and Germany are making triple combos for pennies. We're falling behind. And it's embarrassing.
Kenny Leow
As someone who's been on amlodipine/valsartan for 5 years, I can say this: one pill vs three changed my life. No more pill organizer. No more panic when I travel. Just grab one. 🙌
Kelly Essenpreis
Why do we even have these combos if the individual pills are cheaper? Someone's making money off this. Probably the same people who made the original brand name. It's all rigged
Alexander Williams
The pharmacoeconomic calculus of SPCs is non-linear with respect to adherence metrics. The marginal utility of dose simplification decays asymptotically beyond two-drug combinations. In populations with high baseline adherence, the cost differential renders SPCs economically inefficient. The clinical benefit is statistically significant but clinically marginal for the majority.
Suzanne Mollaneda Padin
If you're on losartan 100mg and HCTZ 25mg separately and it's working, stick with it. But if you're forgetting doses or your BP is still high, ask your doctor about the combo. It's not about being lazy-it's about staying alive. I've helped dozens of patients switch and their numbers dropped within weeks.
Erin Nemo
Just switched to the amlodipine/valsartan combo last month. My copay went from $42 to $12. I didn't even know I could get it cheaper until I checked GoodRx. Thank you for this post!