Generic Drugs: What They Are, How They Save Money, and What to Watch For
When you hear generic drugs, lower-cost versions of brand-name medications that contain the same active ingredients, dosages, and intended uses. Also known as generic medications, they’re the backbone of affordable healthcare in the U.S. and around the world. Most people think generics are just cheaper copies—but they’re not. By law, they must meet the same strict standards as brand drugs. The FDA requires them to deliver the same effect in the body, at the same rate, and with the same safety profile. If your doctor prescribes Lipitor, and you get atorvastatin instead, you’re getting the exact same medicine—just without the fancy packaging or marketing costs.
So why do some people still hesitate? Often, it’s because they’ve been told generics are "inferior"—but that’s not true. The real issue is drug formulary, the list of medications your insurance plan covers and how much you pay for each. Insurance companies push generics because they save them money—and that savings gets passed to you. A brand-name blood pressure pill might cost $150 a month. The generic version? Often under $10. That’s not a trick. That’s how the system works. But here’s the catch: not all generics are created equal in how they’re made. Some use different fillers or coatings, which can affect how quickly the drug is absorbed. For most people, this doesn’t matter. But if you’re on thyroid meds, seizure drugs, or blood thinners, even small changes can cause big problems. That’s why your pharmacist should always check with you before switching.
And don’t forget the role of brand drugs, the original medications developed by pharmaceutical companies and protected by patents. These are the ones with the big ads and the high prices. Once the patent expires, any manufacturer can make the generic. That’s when prices drop—sometimes by 90%. But here’s what no one tells you: sometimes, the brand drug is still cheaper if you use a manufacturer savings program. That’s right. If you’re on a high-cost brand drug, check if the maker offers a copay card or patient assistance program. You might pay less than the generic. It sounds backwards, but it happens. And if you’re switching from brand to generic, make sure your doctor and pharmacist know your full list of meds. Some drugs interact differently with generic versions, especially if you’re on multiple prescriptions.
Then there’s medication safety, the practice of ensuring drugs are used correctly to avoid harm, errors, or dangerous interactions. It’s not just about taking the right pill. It’s about knowing when to question a switch, how to spot counterfeit drugs online, and why your insurance might deny a combo pill even if it’s cheaper overall. You’ll find posts here that break down exactly how antihypertensive combination generics work, how to avoid dangerous interactions with protein-rich meals, and why some side effects fade while others don’t. You’ll see real examples of how people saved hundreds a month by switching—sometimes by accident, sometimes by knowing exactly what to ask for.
Bottom line: generic drugs aren’t a compromise. They’re a smart choice—for your wallet and your health. But they’re not magic. You still need to pay attention. Know your formulary. Ask your pharmacist if the switch is right for you. And never assume that cheaper means safer. The posts below will show you exactly how to navigate this system without getting burned.
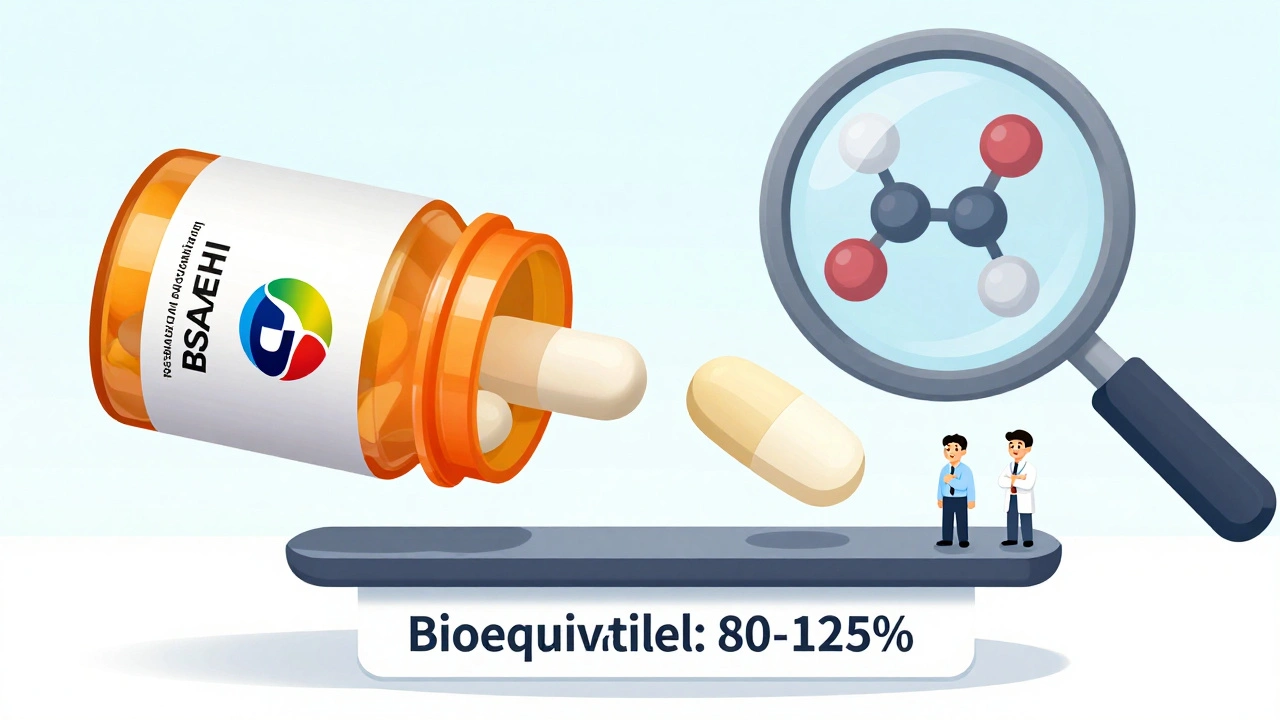
The FDA's ANDA process lets generic drugs reach the market quickly by proving they work the same as brand-name drugs. It saves billions annually and makes medications affordable for millions.
Clinical outcomes data shows generic drugs are just as effective as brand-name medications for nearly all conditions. Providers can confidently prescribe generics to improve adherence, reduce costs, and maintain patient outcomes.
The FDA enforces stricter bioequivalence standards for NTI drugs like warfarin, digoxin, and tacrolimus to prevent dangerous dosing errors. Learn how these rules differ from regular generics and why they matter for patient safety.
Consumer language guides help patients understand that generic drugs are just as safe and effective as brand-name drugs. Learn how plain-language tools are breaking down myths, improving adherence, and saving billions in healthcare costs.
The FDA ensures generic drugs work the same as brand-name versions through strict bioequivalence testing, manufacturing standards, and a rigorous approval process. Over 90% of U.S. prescriptions use generics - all proven safe and effective.
Generic combination products simplify treatment by merging drugs and devices into one unit, improving adherence and cutting costs. They work just like brand-name versions but at 30-80% lower prices - making chronic disease management more accessible.