Narrow Therapeutic Index: What It Means and Why It Matters for Your Medications
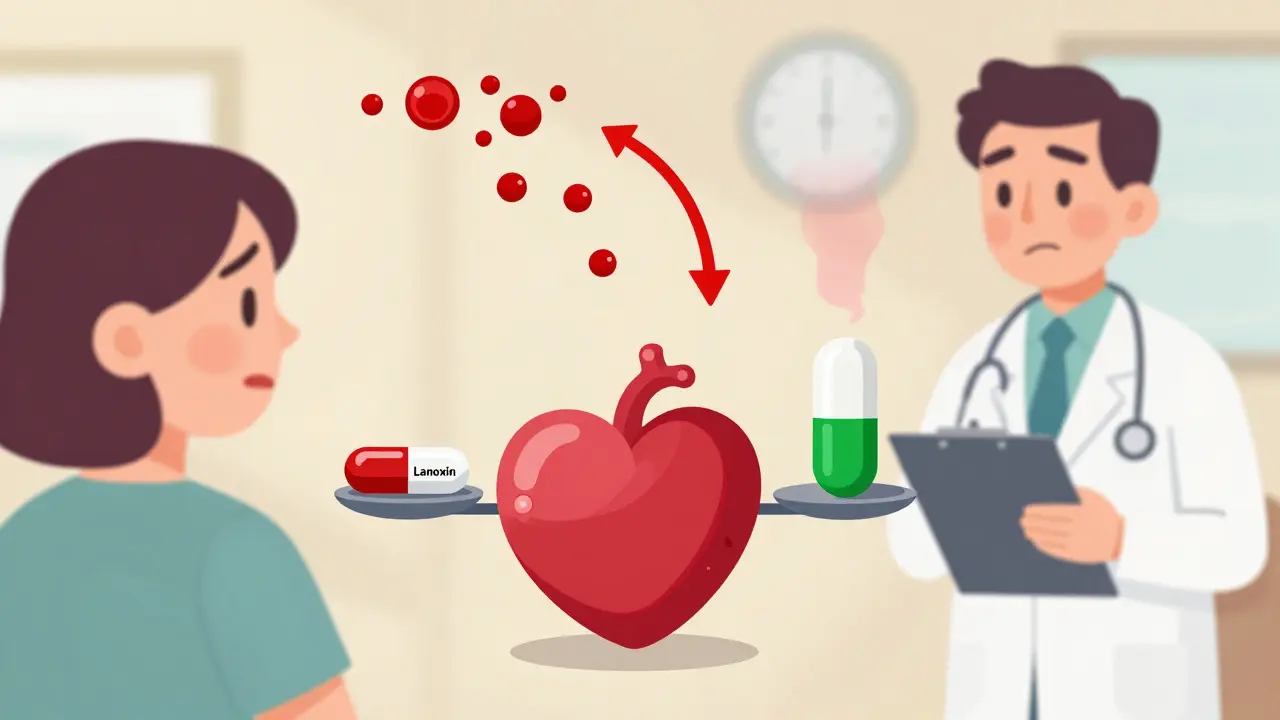
When a drug has a narrow therapeutic index, the range between an effective dose and a toxic one is very small. Also known as a narrow therapeutic window, this means even a slight mistake in dosage can lead to serious side effects—or make the drug useless. Think of it like walking a tightrope: too little and it doesn’t work; too much and you risk poisoning. This isn’t theoretical—it’s why drugs like warfarin, lithium, digoxin, and phenytoin require careful monitoring and exact dosing.
Drugs with a narrow therapeutic index don’t play nice with changes in your body. A change in liver function, kidney health, or even what you eat can throw off how your body handles them. That’s why therapeutic drug monitoring, the practice of measuring drug levels in your blood is often required. It’s not just about labs—it’s about safety. If you’re on one of these drugs, your doctor or pharmacist will likely check your blood levels regularly. And if you switch from brand to generic, you need to know: even though the FDA says generics are equivalent, some patients report differences with narrow index drugs. That’s why bioequivalence isn’t just a regulatory checkbox—it’s a real-world concern.
These drugs also have a higher risk of medication errors, mistakes that happen because dosing is tricky or instructions are unclear. A wrong number on a prescription, a misread label, or even mixing up pills can lead to hospitalization. That’s why understanding your Rx label matters so much. If your pill looks different than last time, ask why. If your pharmacy switches brands without telling you, speak up. You’re not being difficult—you’re protecting yourself.
And it’s not just about the drug itself. Interactions with other meds, supplements, or even grapefruit juice can push a safe dose into the danger zone. Rhodiola, for example, might not seem risky—but when combined with certain antidepressants, it can cause serotonin syndrome. The same logic applies here: a small change, big consequence. That’s why knowing your full medication list and sharing it with every provider is non-negotiable.
There’s no magic fix for narrow therapeutic index drugs. But you can control your part. Keep a written log of doses and symptoms. Use a pill organizer with clear labels. Never skip a dose to "catch up"—that’s when levels get unstable. And if you feel off—dizzy, confused, nauseous, or unusually tired—don’t wait. These could be early signs your drug level is too high.
The posts below cover exactly these kinds of real-life risks and protections. You’ll find guides on how to read your prescription label, why generic combinations sometimes need extra caution, how to avoid dangerous drug interactions, and what to do when your medication changes. These aren’t abstract ideas—they’re the tools you need to stay safe when you’re on a drug that doesn’t forgive mistakes.
Digoxin generics may be bioequivalent on paper, but small differences in absorption can cause toxicity or treatment failure. Learn why strict monitoring and avoiding unnecessary switches are critical for patient safety.
The FDA enforces stricter bioequivalence standards for NTI drugs like warfarin, digoxin, and tacrolimus to prevent dangerous dosing errors. Learn how these rules differ from regular generics and why they matter for patient safety.
Generic medications save money but aren't always identical in how they affect your body. For some drugs, even small differences in absorption can cause serious side effects-especially for people on thyroid, seizure, or blood-thinning meds.